Vascular Structure Identification in Intraoperative 3D Contrast-Enhanced Ultrasound Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Image Dataset
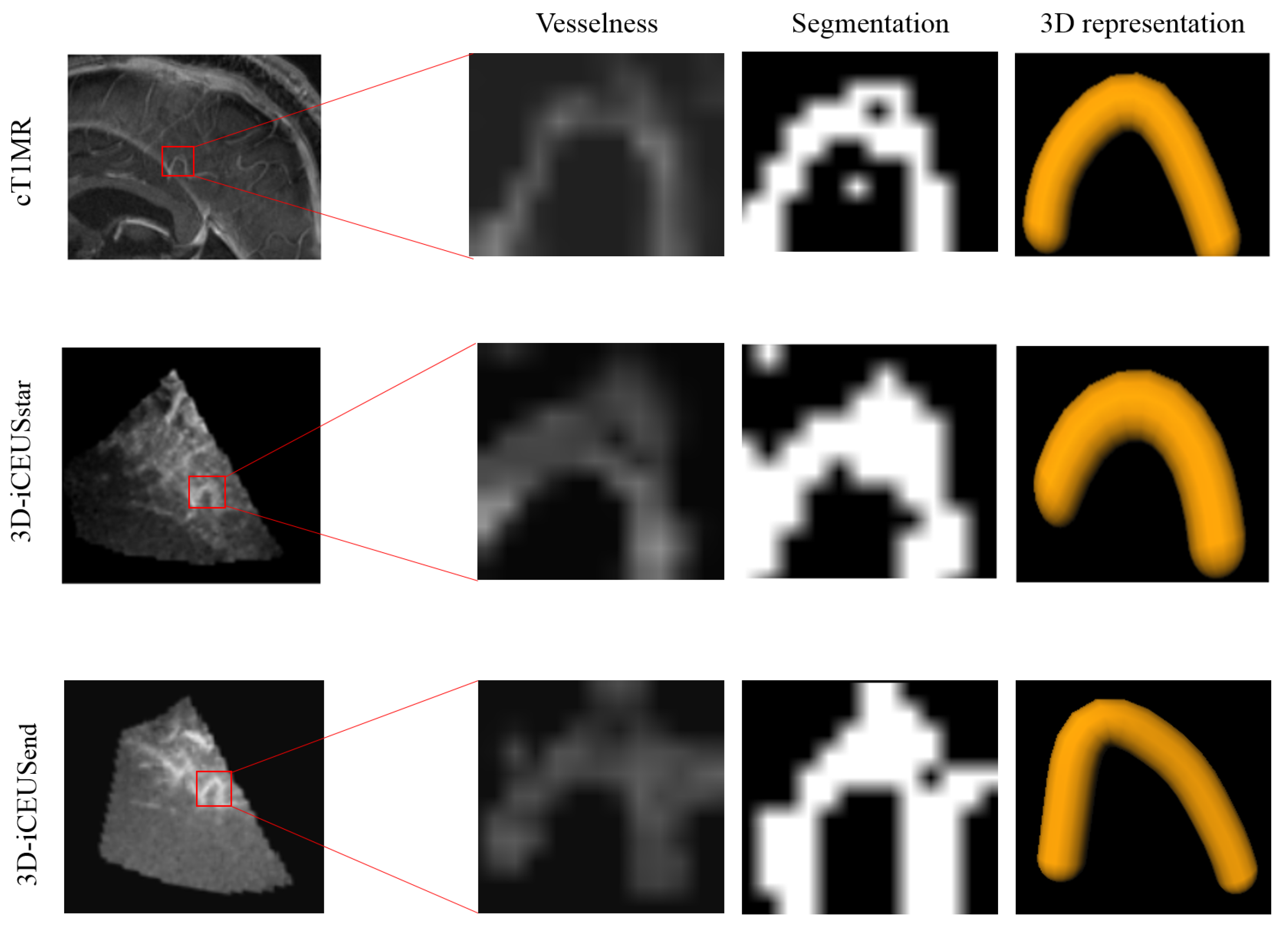
2.2. Vascular Structure Segmentation
2.3. Vascular Structure Identification
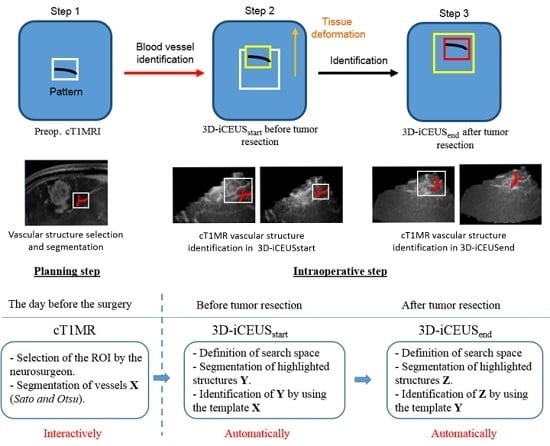
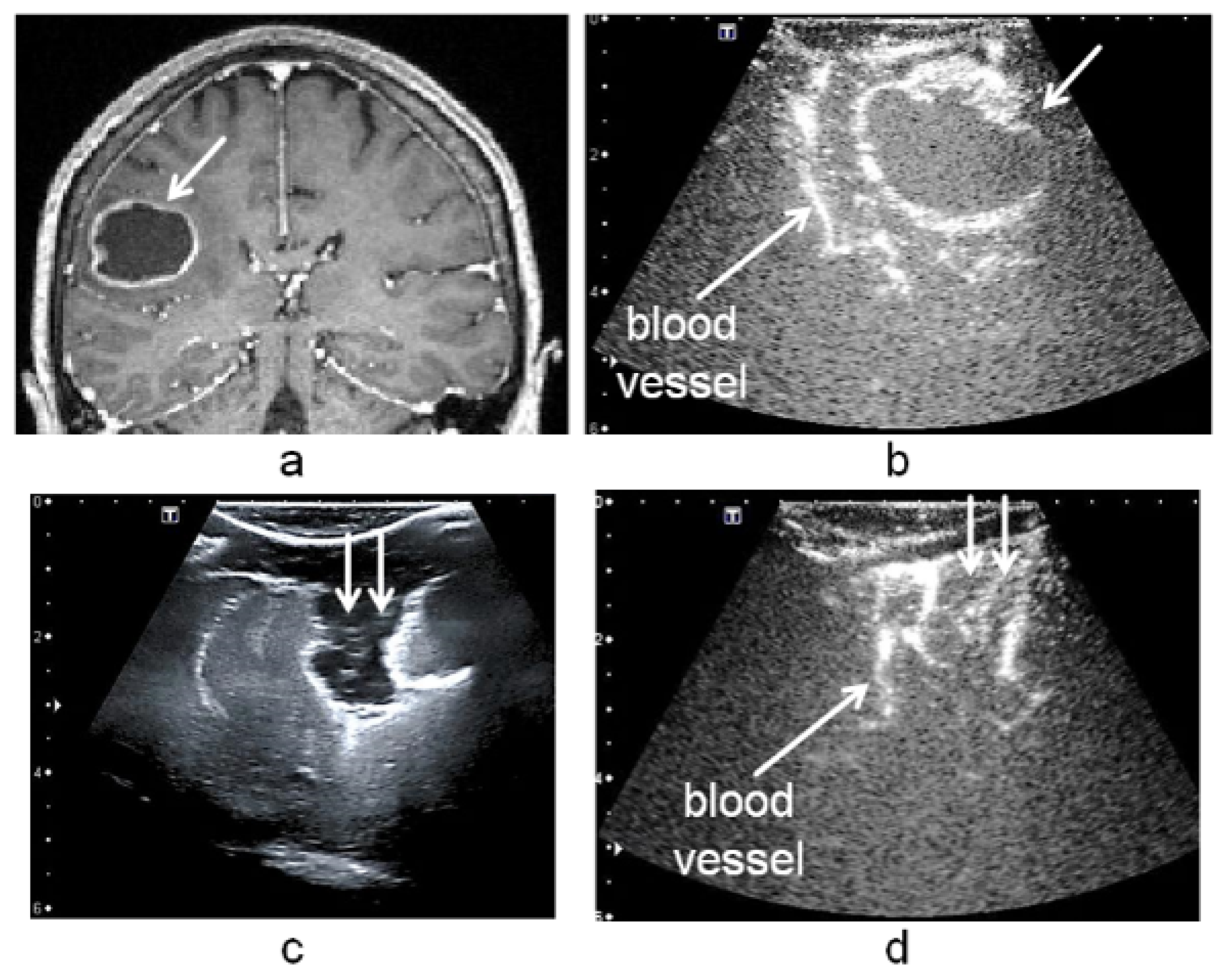
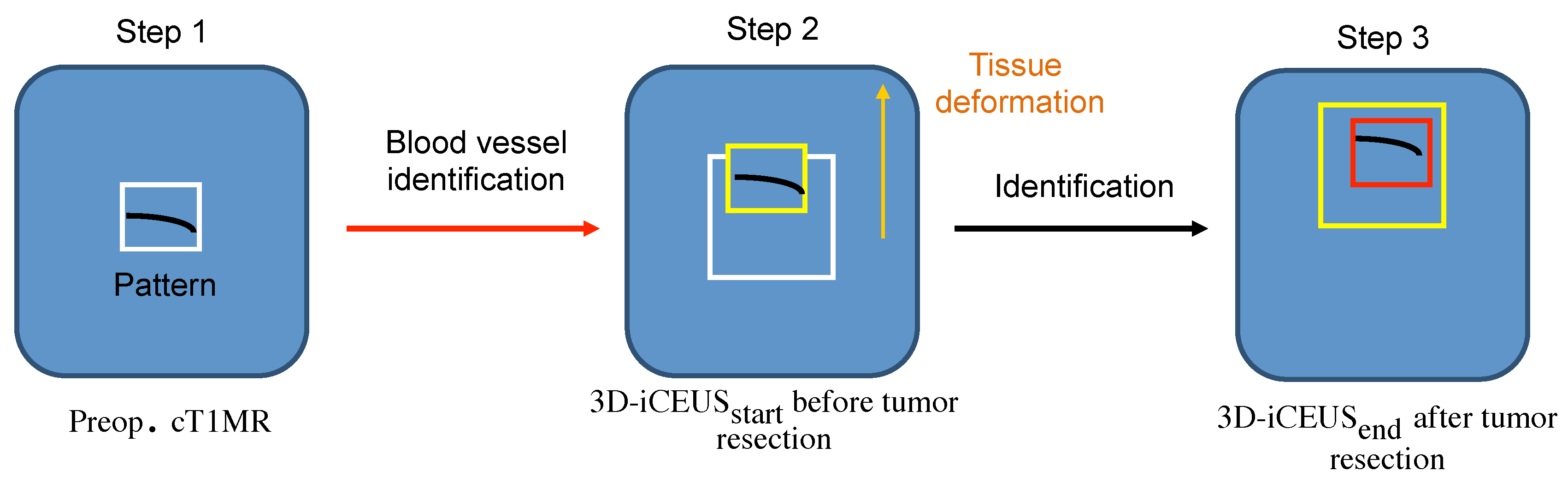
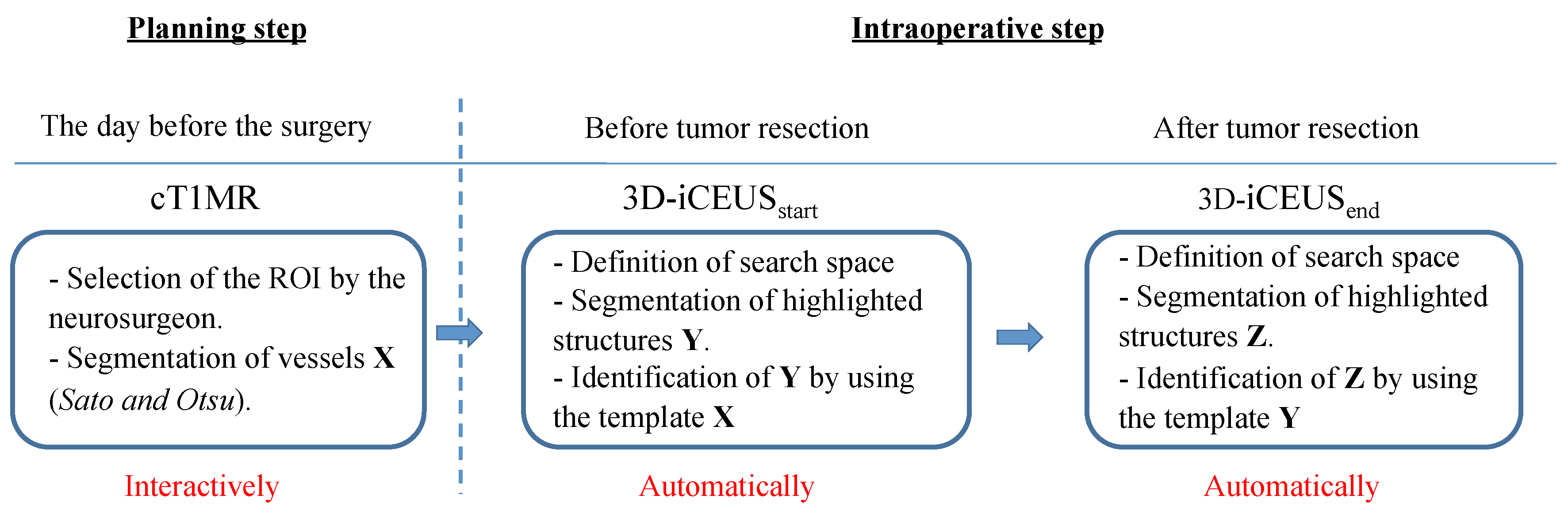
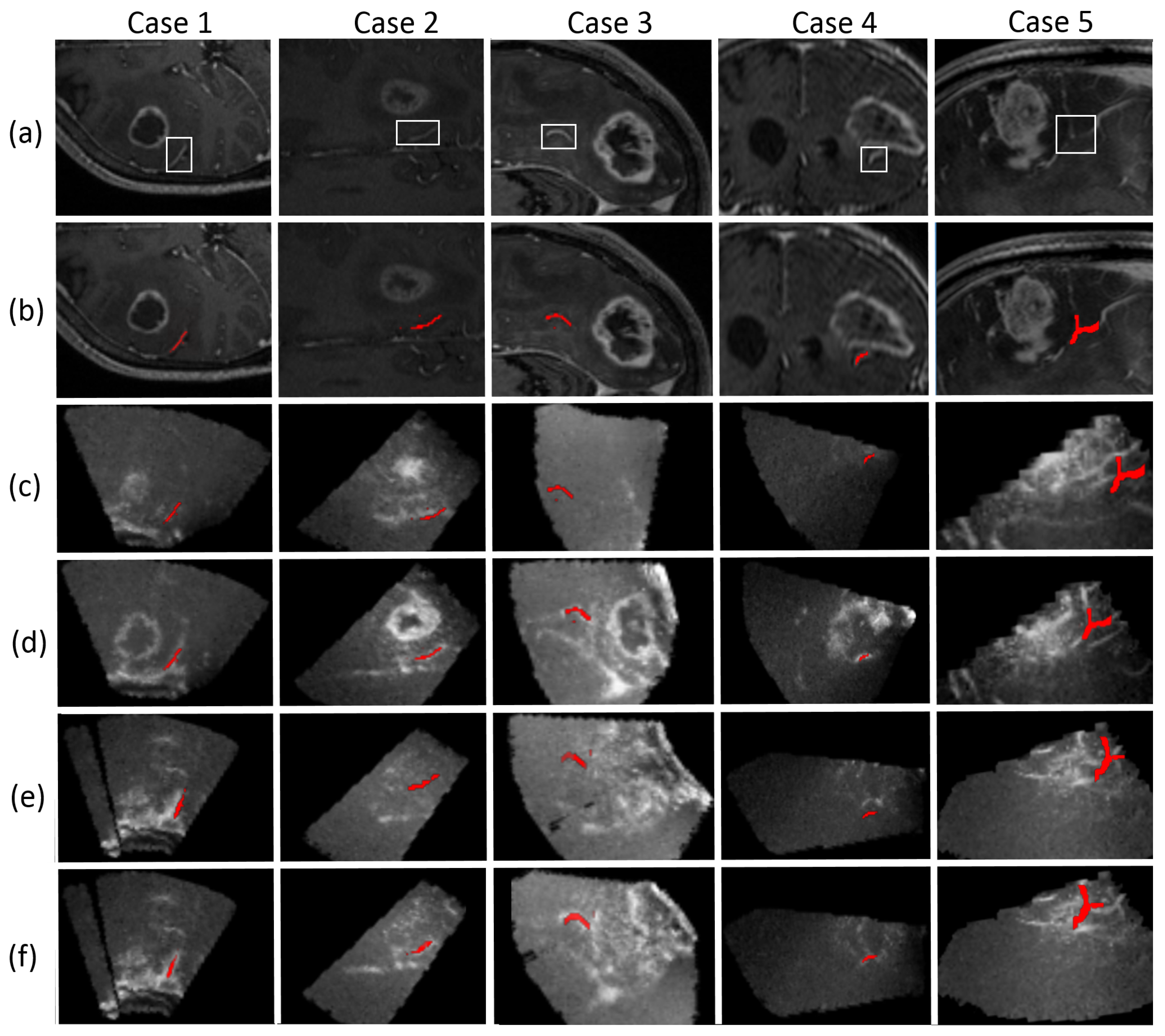
- Step 1: Selecting a vascular segment pattern in cT1MRInteraction with the application in the operating room has to be limited because of sterilization constraints and restricted time. Due to this, during the operation planning, the user delineates interactively a region of interest including a blood vessel near to the tumor in the cT1MR data. The vascular structure is segmented using the method described in Section 2.2. It performs well because the blood vessels are enhanced in the cT1MR data due to the contrast agent, and any other anatomical structure represented with similar intensities is included in the region of interest. The segmented blood vessel represents the pattern (white frame, Step 1, Figure 3) that is searched for in the 3D-iCEUS and 3D-iCEUS data.
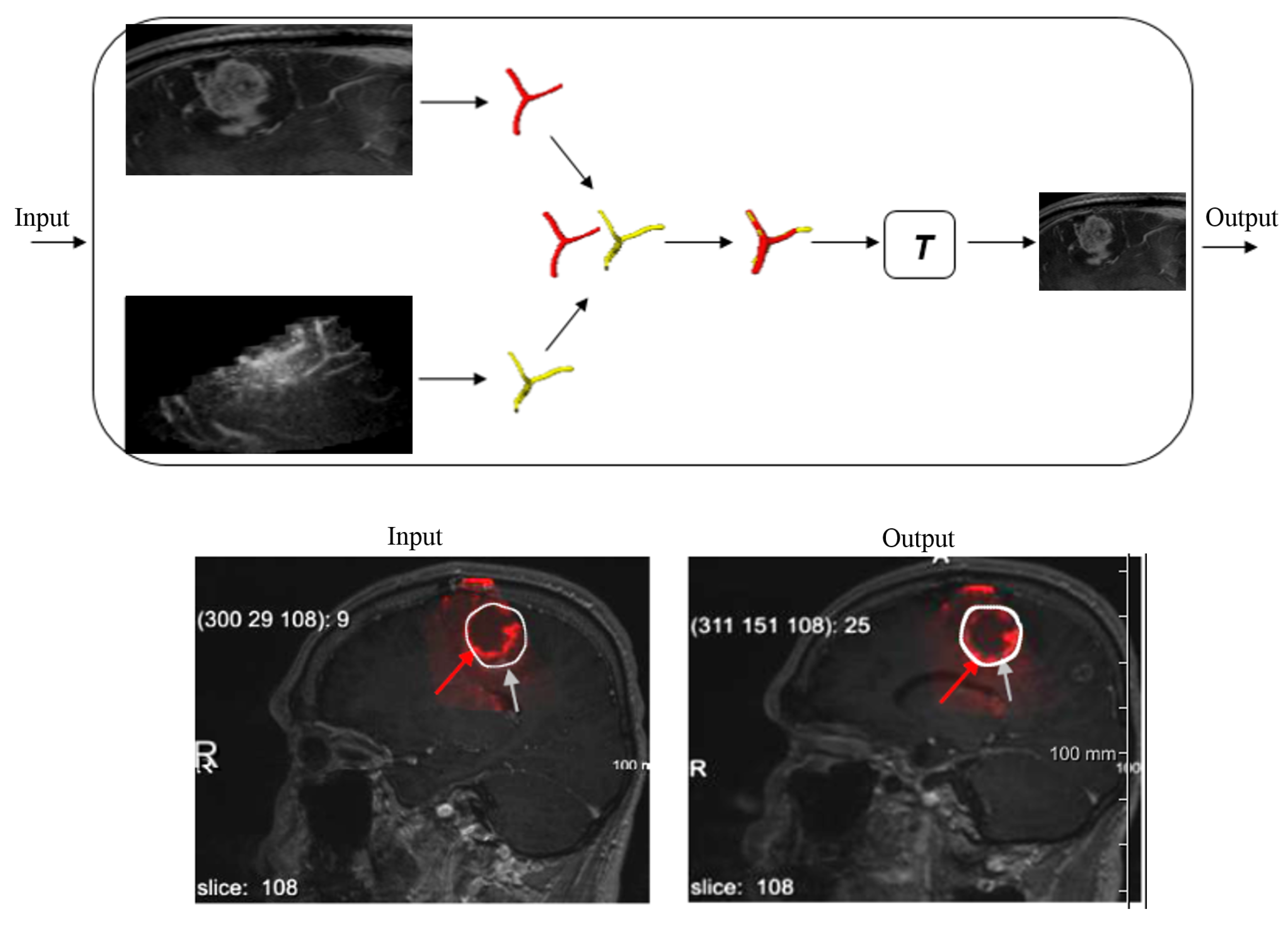
- Step 2: Blood vessel identification in 3D-iCEUSThe pattern is firstly searched in the 3D-iCEUS data acquired before resection. In order to reduce the computing time, the search space (large white frame, Step 2, Figure 3) is smaller than the entire 3D-iCEUS, but large enough to take the tissue deformations into account. It has twice the volume of the region of interest defined in the cT1MR data, and is centered on the same image position. The enhanced structures in this region are segmented and then a rigid registration method is used to find the sample in the 3D-iCEUS data (yellow frame, Step 2, Figure 3) which corresponds best to the pattern. A rigid transformation is sufficient here, since the goal is the identification of the position of the blood vessel in the 3D-iCEUS data, which looks like the vascular segment pattern selected in the cT1MR data. The blood vessel detected in the 3D-iCEUS then becomes the new pattern, which has to be identified in the 3D-iCEUS data after resection.
- Step 3: Blood vessel identification in the 3D-iCEUS
2.4. Validation
3. Results
4. Discussion
4.1. Visual Validation
4.2. Quantitative Validation
4.3. Limitations and Future Improvements
4.3.1. Image Quality
4.3.2. Misidentification of Vascular Structures
4.3.3. Vascular Structures Segmentation
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Unsgaard, G.; Rygh, O.; Selbekk, T.; Muller, T.; Kolstad, F.; Lindseth, F.; Nagelhus Hernes, T. Intra-operative 3D ultrasound in neurosurgery. Acta Neurochir. 2006, 148, 235–253. [Google Scholar] [CrossRef] [PubMed]
- Unsgaard, G.; Selbekk, T.; Muller, T.; Ommedal, S.; Torp, S.; Myhr, G.; Bang, J.; Nagelhus Hernes, T. Ability of navigated 3D ultrasound to delineate gliomas and metastases—Comparison of image interpretations with histopathology. Acta Neurochir. 2005, 147, 1259–1269. [Google Scholar] [CrossRef] [PubMed]
- Selbekk, T.; Jakola, A.; Solheim, O.E.A. Ultrasound imaging in neurosurgery: Approaches to minimize surgically induced image artefacts for improved resection control. Acta Neurochir. 2013, 155, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Solheim, O.; Selbekk, T.; Jakola, A.; Unsgard, G. Ultrasound-guided operations in unselected high-grade gliomas-overall results, impact of image quality and patient selection. Acta Neurochir. 2010, 152, 1873–1886. [Google Scholar] [CrossRef] [PubMed]
- Selbekk, T.; Jakola, A.; Solheim, O.; Johansen, T.; Lindseth, F.; Reinertsen, I.; Unsgard, G. Ultrasound imaging in neurosurgery: approaches to minimize surgically induced image artefacts for improved resection control. Acta Neurochir. 2013, 155, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Trantakis, C.; Meixensberger, J.; Lindner, D.; Straub, G.; Grunst, G.; Schmidtgen, A.; Arnold, S. Iterative neuronavigation using 3D ultrasound. A feasibilty study. Neurol. Res. 2002, 24, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Lindner, D.; Trantakis, C.; Renner, C.; Arnold, S.; Schmitgen, A.; Schneider, J.; Meixensberger, J. Application of Intraoperative 3D Ultrasound During Navigated Tumor Resection. Minim. Invasive Neurosurg. 2006, 49, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Maurer, C.R.; Hill, D.L.G.; Maciunas, R.J.; Barwise, J.A.; Fitzpatrick, J.M.; Wang, M.Y. Medical Image Computing and Computer-Assisted Interventation. In Proceedings of the MICCAI’98: First International Conference, Cambridge, MA, USA, 11–13 October 1998; pp. 51–62.
- Letteboer, M.; Willems, P.; Viergever, M.; Niessen, W. Brain shift estimation in image-guided neurosurgery using 3-D ultrasound. IEEE Trans. Biomed. Eng. 2005, 52, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.; Wu, Z.; Hartov, A.; Roberts, D.W.; Paulsen, K.D. Mutual-information-based image to patient re-registration using intraoperative ultrasound in image-guided neurosurgery. Med. Phys. 2008, 35, 4612–4624. [Google Scholar] [CrossRef] [PubMed]
- Coupe, P.; Hellier, P.; Morandi, X.; Barillot, C. 3D Rigid Registration of Intraoperative Ultrasound and Preoperative MR Brain Images Based on Hyperechogenic Structures. Int. J. Biomed. Imaging 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Fuerst, B.; Wein, W.; Muller, M.; Navab, N. Automatic ultrasound-MRI registration for neurosurgery using the 2D and 3D {LC2} Metric. Med. Image Anal. 2014, 18, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Comeau, R.; Sadikot, A.; Fenster, A.; Peters, T. Intraoperative ultrasound for guidance and tissue shift correction in image-guided neurosurgery. Med. Phys. 2000, 27, 787–800. [Google Scholar] [CrossRef] [PubMed]
- Reinertsen, I.; Lindseth, F.; Unsgaard, G.; Collins, D. Clinical validation of vessel-based registration for correction of brain-shift. Med. Image Anal. 2007, 11, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Hartov, A.; Roberts, D.; Paulsen, K. A comparative analysis of coregistered ultrasound and magnetic resonance imaging in neurosurgery. Neurosurgery 2008, 62, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Ferrant, M.; Nabavi, A.; Macq, B.; Jolesz, F.; Kikinis, R.; Warfield, S. Registration of 3-D intraoperative MR images of the brain using a finite-element biomechanical model. IEEE Trans. Med. Imaging. 2001, 20, 1384–1397. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, D.; Barratt, D.; Blackall, J.; Chan, C.; Edwards, P.; Rhode, K.; Penney, G.; McClelland, J.; Hill, D. Tissue deformation and shape models in image-guided interventions: A discussion paper. Med. Image Anal. 2005, 9, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Reinertsen, I.; Lindseth, F.; Askeland, C.; Iversen, D.H.; Unsgard, G. Intra-operative correction of brain-shift. Acta Neurochir. 2014, 156, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.; Wilkening, W.; Ermert, H.; Engelhardt, M.; Schmieder, K.; Krogias, C.; Eyding, J. Intraoperative contrast enhanced perfusion imaging of cerebral tumors. In Proceedings of the 2005 IEEE Ultrasonics Symposium, Rotterdam, The Netherlands, 18–21 September 2005; Volume 2, pp. 743–746.
- Kanno, H.; Ozawa, Y.; Sakata, K.; Sato, H.; Tanabe, Y.; Shimizu, N.; Yamamoto, I. Intraoperative power Doppler ultrasonography with a contrast-enhancing agent for intracranial tumors. J. Neurosurg. 2005, 102, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Prada, F.; Perin, A.; Martegani, A.; Aiani, L.; Solbiati, L.; Lamperti, M.; Casali, C.; Legnani, F.; Mattei, L.; Saladino, A.; et al. Intraoperative contrast-enhanced ultrasound for brain tumor surgery. Neurosurgery 2014, 74, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Holscher, T.; Ozgur, B.; Singel, S.; Wilkening, W.; Mattrey, R.; Sang, H. Intraoperative ultrasound using phase inversion harmonic imaging: first experiences. Neurosurgery 2007, 60, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Prada, F.; Bene, M.; Saini, M.; Ferroli, P.; DiMeco, F. Intraoperative cerebral angiosonography with ultrasound contrast agents: How I do it. Acta Neurochir. 2015, 157, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- Hyvelin, J.M.; Greis, C.; Gaud, E.; Costa, M.; Helbert, A.; Bussat, P.; Bettinger, T.; Frinking, P. Characteristics and echogenicity of clinical ultrasound contrast agents: An in vitro and in vivo comparison study. In Proceedings of the 21 European Symposium on Ultrasound Contrast Imaging, An ICUS Conference, Erasmus MC Rotterdam, Rotterdam, The Netherlands, 21–22 January 2016; pp. 5–8.
- Gill, J.; Ladak, H.; Steinman, D.; Fenster, A. Accuracy and variability assessment of a semiautomatic technique for segmentation of the carotid arteries from three-dimensional ultrasound images. Med. Phys. 2000, 27, 1333–1342. [Google Scholar] [CrossRef] [PubMed]
- Chalopin, C.; Krissian, K.; Meixensberger, J.; Muns, A.; Arlt, F.; Lindner, D. Evaluation of a semi-automatic segmentation algorithm in 3D intraoperative ultrasound brain angiography. Biomed. Tech. 2013, 58, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Otsu, N. A Threshold Selection Method from Gray-Level Histograms. IEEE Trans. Syst. Man Cybern. 1979, 9, 62–66. [Google Scholar]
- Yoshinobu, S.; Shin, N.; Atsumi, H.; Thomas, K.; Guido, G.; Shigeyuki, Y.; Ron, K. CVRMed-MRCAS’97: First Joint Conference Computer Vision. In Proceedings of the Virtual Reality and Robotics in Medicine and Medical Robotics and Computer-Assisted Surgery, Grenoble, France, 19–22 March 1997; pp. 213–222.
- Sato, Y.; Nakajima, S.; Shiraga, N.; Atsumi, H.; Yoshida, S.; Koller, T.; Gerig, G.; Kikinis, R. Three-dimensional multi-scale line filter for segmentation and visualization of curvilinear structures in medical images. Med. Image Anal. 1998, 2, 143–168. [Google Scholar] [CrossRef]
- Luu, H.M.; Klink, C.; Moelker, A.; Niessen, W.; van Walsum, T. Quantitative evaluation of noise reduction and vesselness filters for liver vessel segmentation on abdominal CTA images. Phys. Med. Biol. 2015, 60, 3905–3926. [Google Scholar] [CrossRef] [PubMed]
- Drechsler, K.; Laura, C.O. Comparison of vesselness functions for multiscale analysis of the liver vasculature. In Proceedings of the 2010 10th IEEE International Conference on Information Technology and Applications in Biomedicine (ITAB), Corfu, Greece, 3–5 November 2010; pp. 1–5.
- Andronache, A.; von Siebenthal, M.; Székely, G.; Cattin, P. Non-rigid registration of multi-modal images using both mutual information and cross-correlation. Med. Image Anal. 2008, 12, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Pluim, J.; Maintz, J.; Viergever, M. Mutual-information-based registration of medical images: A survey. IEEE Trans. Med. Imaging 2003, 22, 986–1004. [Google Scholar] [CrossRef] [PubMed]
- Hodneland, E.; Lundervold, A.; Rorvik, J.; Munthe-Kaas, A.Z. Normalized gradient fields for nonlinear motion correction of DCE-MRI time series. Comput. Med. Imaging Graph. 2014, 38, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Haber, E.; Modersitzki, J. Bildverarbeitung für die Medizin 2005: Algorithmen—Systeme—Anwendungen Proceedings des Workshops vom 13.–15. März 2005 in Heidelberg; Springer Berlin Heidelberg: Heidelberg, Germany, 2005; pp. 350–354. [Google Scholar]
- Bogush, R.; Maltsev, S.; Ablameyko, S.; Uchida, S.; Kamata, S. An efficient correlation computation method for binary images based on matrix factorisation. In Proceedings of the Sixth International Conference on Document Analysis and Recognition, Seattle, WA, USA, 10–13 September 2001; pp. 312–316.
- Chanwimaluang, T.; Fan, G.; Fransen, S. Hybrid retinal image registration. IEEE Trans. Inf. Technol. Biomed. 2006, 10, 129–142. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Qiao, G.; Zhang, R.; Zong, G. Characteristics of Independence on Image Gray Level in NCCO Applications. In Proceedings of the International Conference on Information Technology and Computer Science (ITCS 2009), Kiev, Ukraine, 25–26 July 2009; Volume 2, pp. 275–278.
- Crabb, M.G.; Davidson, J.L.; Little, R.; Wright, P.; Morgan, A.R.; Miller, C.A.; Naish, J.H.; Parker, G.J.M.; Kikinis, R.; McCann, H.; et al. Mutual information as a measure of image quality for 3D dynamic lung imaging with EIT. Physiol. Meas. 2014, 35, 863. [Google Scholar] [CrossRef] [PubMed]
- Müns, A.; Meixensberger, J.; Arnold, S.; Schmitgen, A.; Arlt, F.; Chalopin, C.; Lindner, D. Integration of a 3D ultrasound probe into neuronavigation. Acta Neurochir. 2011, 153, 1529–1533. [Google Scholar] [CrossRef] [PubMed]
- Chalopin, C.; Lindenberg, R.; Arlt, F.; Muns, A.; Meixensberger, J.; Lindner, D. Brain tumor enhancement revealed by 3D intraoperative ultrasound imaging in a navigation system. Biomed. Eng./Biomed. Tech. 2012, 57, 468–471. [Google Scholar] [CrossRef]
- Lowe, D.G. Object recognition from local scale-invariant features. In Proceedings of the Seventh IEEE International Conference on Computer Vision, Kerkyra, Greece, 20–27 September 1999; Volume 2, pp. 1150–1157.
- Lowe, D.G. Distinctive Image Features from Scale-Invariant Keypoints. Int. J. Comput. Vis. 2004, 60, 91–110. [Google Scholar] [CrossRef]
- Ghassabi, Z.; Shanbehzadeh, J.; Sedaghat, A.; Fatemizadeh, E. An efficient approach for robust multimodal retinal image registration based on UR-SIFT features and PIIFD descriptors. EURASIP J. Image Video Process. 2013, 2013, 1–16. [Google Scholar] [CrossRef]
- Chen, J.; Tian, J. Real-time multi-modal rigid registration based on a novel symmetric-SIFT descriptor. Progress Natural Sci. 2009, 19, 643–651. [Google Scholar] [CrossRef]
- Cruz-Aceves, I.; Oloumi, F.; Rangayyan, R.M.; Avina-Cervantes, J.G.; Hernandez-Aguirre, A. Automatic segmentation of coronary arteries using Gabor filters and thresholding based on multiobjective optimization. Biomed. Signal Process. Control 2016, 25, 76–85. [Google Scholar] [CrossRef]
| Patient | Similarity Measure | ROI in cT1MR (voxels) | Blood Vessel Identification in the 3D-iCEUS Using the Pattern from the cT1MR | Blood Vessel Identification in the 3D-iCEUS Using the Pattern from the 3D-iCEUS | ||||
|---|---|---|---|---|---|---|---|---|
| Processing Time (s) | DSI | Hausdorff Distance (mm) | Processing Time (s) | DSI | Hausdorff Distance (mm) | |||
| NGF | 2.8 | 0.89 | 8.083 | 3.5 | 0.824 | 12.207 | ||
| 1 | NMI | 50 × 29 × 8 | 2 | 0.903 | 7.874 | 2.8 | 0.937 | 11.180 |
| NCC | 1.8 | 0.982 | 7.483 | 1.7 | 0.994 | 10.770 | ||
| NGF | 11.1 | 0.645 | 21.772 | 14 | 0.813 | 11.180 | ||
| 2 | NMI | 19 × 37 × 26 | 3.5 | 0.946 | 17.917 | 2.3 | 0.936 | 10.677 |
| NCC | 5.9 | 0.676 | 18.815 | 2.1 | 0.0 * | 14.071 * | ||
| NGF | 3.1 | 0.976 | 5.385 | 1.3 | 0.986 | 12.042 | ||
| 3 | NMI | 35 × 16 × 13 | 2.9 | 0.997 | 5.385 | 0.3 | 0.263 * | 21.237 * |
| NCC | 0.9 | 0.979 | 5.385 | 0.5 | 0.0 * | 22.159 * | ||
| NGF | 5.7 | 0.766 | 12.369 | 1.5 | 0.829 | 9.487 | ||
| 4 | NMI | 15 × 17 × 22 | 0.7 | 0.937 | 8.124 | 0.7 | 0.925 | 8.602 |
| NCC | 0.9 | 0.839 | 9.274 | 7.4 | 0.825 | 9.487 | ||
| NGF | 2.1 | 0.748 | 13.403 | 13 | 0.763 | 29.172 | ||
| 5 | NMI | 61 × 55 × 8 | 2.2 | 0.422 * | 28.792 * | 4.9 | 0.38 | 34.015 * |
| NCC | 1.2 | 0.408 * | 29.682 * | 6.7 | 0.674 | 32.016 | ||
| NGF | 0.4 | 0.0 * | 22.023 * | - | - | - | ||
| 6 | NMI | 8 × 39 × 26 | 1.8 | 0.832 | 9.110 | 4.9 | 0.98 | 10.863 |
| NCC | 2.4 | 0.832 | 9.110 | 16.2 | 0.913 | 10.863 | ||
| NGF | 17.6 | 0.953 | 28.547 | 56.6 | 1 | 17.234 | ||
| 7 | NMI | 49 × 56 × 29 | 11.3 | 0.827 | 29.653 | 30.2 | 0.051 * | 19.519 * |
| NCC | 9.1 | 0.983 | 28.530 | 8.8 | 0.0 * | 19.519 * | ||
| NGF | 3.2 | 0.988 | 4.690 | 8.3 | 0.849 | 10.050 | ||
| 8 | MI | 32 × 14 × 19 | 2.9 | 0.031 * | 17.720 * | - | - | - |
| NCC | 1.3 | 0.097 * | 15.524 * | - | - | - | ||
| NGF | 3.1 | 0.988 | 14.000 | 4.1 | 0.879 | 14.000 | ||
| 9 | NMI | 31 × 22 × 22 | 2.5 | 0.475 * | 24.083 * | - | - | - |
| NCC | 3.5 | 0.458 * | 25.729 * | - | - | - | ||
| NGF | 2.7 | 0.952 | 2.449 | 1.5 | 0.961 | 3.162 | ||
| 10 | NMI | 12 × 18 × 12 | 0.7 | 0.818 | 2.500 | 0.7 | 0.0 * | 8.464 * |
| NCC | 2.4 | 0.952 | 2.449 | 1.8 | 0.0 * | 8.718 * | ||
| Comparative Studies | Mean DSI (Algorithm, Expert) Computed after Registration in the: | Mean Hausdorff Distances in mm (Algorithm, Expert) Computed after Registration in the: | ||
|---|---|---|---|---|
| 3D-iCEUS | 3D-iCEUS | 33D-iCEUS | 3D-iCEUS | |
| NGF vs. Expert | 0.870 | 0.868 | 13.272 | 13.170 |
| NMI vs. Expert | 0.838 | 0.832 | 15.116 | 15.570 |
| NCC vs. Expert | 0.815 | 0.852 | 15.198 | 15.950 |
| Similarity Measure | cT1MR − 3D-iCEUS | 3D-iCEUS − 3D-iCEUS |
|---|---|---|
| NGF | 6.1 | 12.8 |
| NMI | 3.5 | 3.1 |
| NCC | 3.2 | 8.0 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilunga-Mbuyamba, E.; Avina-Cervantes, J.G.; Lindner, D.; Cruz-Aceves, I.; Arlt, F.; Chalopin, C. Vascular Structure Identification in Intraoperative 3D Contrast-Enhanced Ultrasound Data. Sensors 2016, 16, 497. https://doi.org/10.3390/s16040497
Ilunga-Mbuyamba E, Avina-Cervantes JG, Lindner D, Cruz-Aceves I, Arlt F, Chalopin C. Vascular Structure Identification in Intraoperative 3D Contrast-Enhanced Ultrasound Data. Sensors. 2016; 16(4):497. https://doi.org/10.3390/s16040497
Chicago/Turabian StyleIlunga-Mbuyamba, Elisee, Juan Gabriel Avina-Cervantes, Dirk Lindner, Ivan Cruz-Aceves, Felix Arlt, and Claire Chalopin. 2016. "Vascular Structure Identification in Intraoperative 3D Contrast-Enhanced Ultrasound Data" Sensors 16, no. 4: 497. https://doi.org/10.3390/s16040497