Connexin 43 Plays a Role in Pulmonary Vascular Reactivity in Mice
Abstract
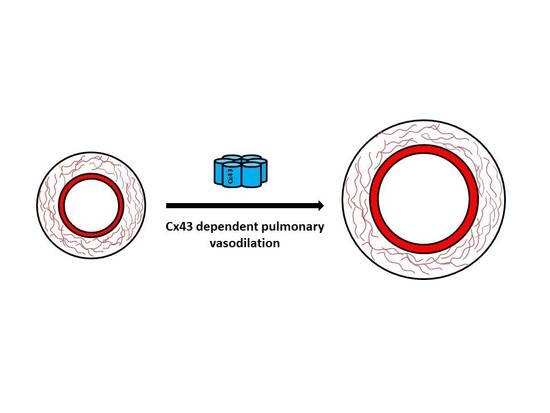
:1. Introduction
2. Results
2.1. Gene Expression of Connexins in Pulmonary Arteries from Cx43 heterozygous Mice
2.2. Pulmonary Arterial Contractile Responses
2.3. Pulmonary Arterial Relaxation Responses
2.4. Gene Expression of Bone Morphogenetic Protein Receptor Type II, Tryptophan Hydroxylase 1, and Endothelial Nitric Oxide Synthase in Pulmonary Arteries from Cx43 Heterozygous Mice
2.5. Effects of Hypoxia on Pulmonary Vascular Contractility in Male Cx43 Heterozugous Mice
2.6. Effects of Hypoxia on Expression of Cx43 in Mouse Lung and Pulmonary Artery
2.7. Effects of Hypoxia on Gene Expression in Pulmonary Arteries Derived from WT and Cx43+/− Mice
3. Discussion
4. Materials and Methods
4.1. Ethical Statement
4.2. Animals
4.3. Genotyping
4.4. Induction of Hypoxia
4.5. Tissue Preparation
4.6. Wire Myography Studies
4.7. Quantitative Real Time PCR (qPCR)
4.8. Immunofluorescence Staining
4.9. Statistical Analysis
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Hoeper, M.M.; Bogaard, H.J.; Condliffe, R.; Frantz, R.; Khanna, D.; Kurzyna, M.; Langleben, D.; Manes, A.; Satoh, T.; Torres, F. Definitions and Diagnosis of Pulmonary Hypertension. J. Am. Coll. Cardiol. 2013, 62, D42–D50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benza, R.L.; Miller, D.P.; Barst, R.J.; Badesch, D.B.; Frost, A.E.; McGoon, M.D. An Evaluation of Long-Term Survival from Time of Diagnosis in Pulmonary Arterial Hypertension from the REVEAL Registry. Chest 2012, 142, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Dempsie, Y.; MacLean, M.R. The Influence of Gender on the Development of Pulmonary Arterial Hypertension. Exp. Physiol. 2013, 98, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Dempsie, Y.; Martin, P.; Upton, P.D. Connexin-Mediated Regulation of the Pulmonary Vasculature. Biochem. Soc. Trans. 2015, 43, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Eddahibi, S.; Guignabert, C.; Barlier-Mur, A.M.; Dewachter, L.; Fadel, E.; Dartevelle, P.; Humbert, M.; Simonneau, G.; Hanoun, N.; Saurini, F.; et al. Cross Talk between Endothelial and Smooth Muscle Cells in Pulmonary Hypertension: Critical Role for Serotonin-Induced Smooth Muscle Hyperplasia. Circulation 2006, 113, 1857–1864. [Google Scholar] [CrossRef] [PubMed]
- MacLean, M.R.; Dempsie, Y. The serotonin hypothesis of pulmonary hypertension revisited. In Membrane Receptors, Channels and Transporters in Pulmonary Circulation; Humana Press: Totowa, NJ, USA, 2010; pp. 309–322. [Google Scholar]
- Xu, W.; Kaneko, F.T.; Zheng, S.; Comhair, S.A.; Janocha, A.J.; Goggans, T.; Thunnissen, F.B.; Farver, C.; Hazen, S.L.; Jennings, C. Increased Arginase II and Decreased NO Synthesis in Endothelial Cells of Patients with Pulmonary Arterial Hypertension. FASEB J. 2004, 18, 1746–1748. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.E.; Evans, W.H. Incorporation of Connexins into Plasma Membranes and Gap Junctions. Cardiovasc. Res. 2004, 62, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, X.F.; Duling, B.R. Gap Junctions in the Control of Vascular Function. Antioxid. Redox Signal. 2009, 11, 251–266. [Google Scholar] [CrossRef] [PubMed]
- Brisset, A.C.; Isakson, B.E.; Kwak, B.R. Connexins in Vascular Physiology and Pathology. Antioxid. Redox Signal. 2009, 11, 267–282. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, S.; Isakson, B.; Locke, D. Biological and Biophysical Properties of Vascular Connexin Channels. Int. Rev. Cell Mol. Biol. 2009, 278, 69–118. [Google Scholar] [PubMed]
- Sosinsky, G.E.; Boassa, D.; Dermietzel, R.; Duffy, H.S.; Laird, D.W.; MacVicar, B.; Naus, C.C.; Penuela, S.; Scemes, E.; Spray, D.C. Pannexin Channels are Not Gap Junction Hemichannels. Channels 2011, 5, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Lohman, A.W.; Billaud, M.; Straub, A.C.; Johnstone, S.R.; Best, A.K.; Lee, M.; Barr, K.; Penuela, S.; Laird, D.W.; Isakson, B.E. Expression of Pannexin Isoforms in the Systemic Murine Arterial Network. J. Vasc. Res. 2012, 49, 405–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Billaud, M.; Chiu, Y.H.; Lohman, A.W.; Parpaite, T.; Butcher, J.T.; Mutchler, S.M.; DeLalio, L.J.; Artamonov, M.V.; Sandilos, J.K.; Best, A.K.; et al. A Molecular Signature in the pannexin1 Intracellular Loop Confers Channel Activation by the alpha1 Adrenoreceptor in Smooth Muscle Cells. Sci. Signal. 2015, 8, ra17. [Google Scholar] [CrossRef] [PubMed]
- Tsang, H.; Leiper, J.; Lao, K.H.; Dowsett, L.; Delahaye, M.W.; Barnes, G.; Wharton, J.; Howard, L.; Iannone, L.; Lang, N.N. Role of Asymmetric Methylarginine and Connexin 43 in the Regulation of Pulmonary Endothelial Function. Pulm. Circ. 2013, 3, 675–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.; Hwangbo, C.; Hu, X.; Kang, Y.; Papangeli, I.; Mehrotra, D.; Park, H.; Ju, H.; McLean, D.L.; Comhair, S.A.; et al. Restoration of Impaired Endothelial Myocyte Enhancer Factor 2 Function Rescues Pulmonary Arterial Hypertension. Circulation 2015, 131, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yin, J.; Nickles, H.T.; Ranke, H.; Tabuchi, A.; Hoffmann, J.; Tabeling, C.; Barbosa-Sicard, E.; Chanson, M.; Kwak, B.R.; et al. Hypoxic Pulmonary Vasoconstriction Requires Connexin 40-Mediated Endothelial Signal Conduction. J. Clin. Investig. 2012, 122, 4218–4230. [Google Scholar] [CrossRef] [PubMed]
- Billaud, M.; Dahan, D.; Marthan, R.; Savineau, J.; Guibert, C. Role of the Gap Junctions in the Contractile Response to Agonists in Pulmonary Artery from Two Rat Models of Pulmonary Hypertension. Respir. Res. 2011, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Mair, K.; MacLean, M.; Morecroft, I.; Dempsie, Y.; Palmer, T. Novel Interactions between the 5-HT Transporter, 5-HT1B Receptors and Rho Kinase in Vivo and in Pulmonary Fibroblasts. Br. J. Pharmacol. 2008, 155, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, C.C.; Du, L.; Chu, D.; Cho, A.J.; Kido, M.; Wolf, P.L.; Jamieson, S.W.; Thistlethwaite, P.A. Induction of Pulmonary Hypertension by an Angiopoietin 1/TIE2/serotonin Pathway. Proc. Natl. Acad. Sci. USA 2003, 100, 12331–12336. [Google Scholar] [CrossRef] [PubMed]
- Morecroft, I.; Dempsie, Y.; Bader, M.; Walther, D.J.; Kotnik, K.; Loughlin, L.; Nilsen, M.; MacLean, M.R. Effect of Tryptophan Hydroxylase 1 Deficiency on the Development of Hypoxia-Induced Pulmonary Hypertension. Hypertension 2007, 49, 232–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gairhe, S.; Bauer, N.N.; Gebb, S.A.; McMurtry, I.F. Serotonin Passes through Myoendothelial Gap Junctions to Promote Pulmonary Arterial Smooth Muscle Cell Differentiation. Am. J. Physiol. Lung Cell Mol. Physiol. 2012, 303, L767–L777. [Google Scholar] [CrossRef] [PubMed]
- Gairhe, S.; Bauer, N.N.; Gebb, S.A.; McMurtry, I.F. Myoendothelial Gap Junctional Signaling Induces Differentiation of Pulmonary Arterial Smooth Muscle Cells. Am. J. Physiol. Lung Cell Mol. Physiol 2011, 301, L527–L535. [Google Scholar] [CrossRef] [PubMed]
- Reaume, A.G.; de Sousa, P.A.; Kulkarni, S.; Langille, B.L.; Zhu, D.; Davies, T.C.; Juneja, S.C.; Kidder, G.M.; Rossant, J. Cardiac Malformation in Neonatal Mice Lacking connexin43. Science 1995, 267, 1831–1834. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.M.; Yuan, H.; Edwards, J.G.; Skayian, Y.; Ochani, K.; Miller, E.J.; Sehgal, P.B. Deletion of STAT5a/b in Vascular Smooth Muscle Abrogates the Male Bias in Hypoxic Pulmonary Hypertension in Mice: Implications in the Human Disease. Mol. Med. 2015, 20, 625–638. [Google Scholar] [PubMed]
- Ma, L.; Chung, W.K. The Genetic Basis of Pulmonary Arterial Hypertension. Hum. Genet. 2014, 133, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Orriols, M.; Gomez-Puerto, M.C.; ten Dijke, P. BMP Type II Receptor as a Therapeutic Target in Pulmonary Arterial Hypertension. Cell. Mol. Life Sci. 2017, 74, 2979–2995. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, X.F.; Lillo, M.A.; Gaete, P.S.; Riquelme, M.A.; Sáez, J.C. Diffusion of Nitric Oxide Across Cell Membranes of the Vascular Wall Requires Specific Connexin-Based Channels. Neuropharmacology 2013, 75, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Looft-Wilson, R.; Billaud, M.; Johnstone, S.; Straub, A.; Isakson, B. Interaction between Nitric Oxide Signaling and Gap Junctions: Effects on Vascular Function. Biochim. Biophys. Acta 2012, 1818, 1895–1902. [Google Scholar] [CrossRef] [PubMed]
- Straub, A.C.; Billaud, M.; Johnstone, S.R.; Best, A.K.; Yemen, S.; Dwyer, S.T.; Looft-Wilson, R.; Lysiak, J.J.; Gaston, B.; Palmer, L.; et al. Compartmentalized Connexin 43 S-nitrosylation/denitrosylation Regulates Heterocellular Communication in the Vessel Wall. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.; Gloe, T.; Pohl, U.; Zahler, S. Nitric Oxide Enhances De Novo Formation of Endothelial Gap Junctions. Cardiovasc. Res. 2003, 60, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Alonso, F.; Boittin, F.X.; Beny, J.L.; Haefliger, J.A. Loss of connexin40 is Associated with Decreased Endothelium-Dependent Relaxations and eNOS Levels in the Mouse Aorta. Am. J. Physiol. Heart Circ. Physiol. 2010, 299, H1365–H1373. [Google Scholar] [CrossRef] [PubMed]
- Kameritsch, P.; Khandoga, N.; Nagel, W.; Hundhausen, C.; Lidington, D.; Pohl, U. Nitric Oxide Specifically Reduces the Permeability of Cx37-containing Gap Junctions to Small Molecules. J. Cell. Physiol. 2005, 203, 233–242. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, R.L.; Bolon, M.L.; Wang, H.X.; Swarbreck, S.; Kidder, G.M.; Simon, A.M.; Tyml, K. Reduction of Electrical Coupling between Microvascular Endothelial Cells by NO Depends on connexin37. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H93–H101. [Google Scholar] [CrossRef] [PubMed]
- Leblais, V.; Delannoy, E.; Fresquet, F.; Bégueret, H.; Bellance, N.; Banquet, S.; Allieres, C.; Leroux, L.; Desgranges, C.; Gadeau, A. Β-Adrenergic Relaxation in Pulmonary Arteries: Preservation of the Endothelial Nitric Oxide-Dependent β2 Component in Pulmonary Hypertension. Cardiovasc. Res. 2007, 77, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Mair, K.; Johansen, A.; Wright, A.; Wallace, E.; MacLean, M. Pulmonary Arterial Hypertension: Basis of Sex Differences in Incidence and Treatment Response. Br. J. Pharmacol. 2014, 171, 567–579. [Google Scholar] [CrossRef] [PubMed]
- Polderman, K.H.; Stehouwer, C.D.; van Kamp, G.J.; Dekker, G.A.; Verheugt, F.W.; Gooren, L.J. Influence of Sex Hormones on Plasma Endothelin Levels. Ann. Intern. Med. 1993, 118, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, T.; Yanagisawa, M.; Iida, K.; Ajisaka, R.; Suzuki, N.; Fujino, M.; Goto, K.; Masaki, T.; Sugishita, Y. Age-and Sex-Related Variation of Plasma Endothelin-1 Concentration in Normal and Hypertensive Subjects. Am. Heart J. 1992, 123, 1092–1093. [Google Scholar] [CrossRef]
- Ergul, A.; Shoemaker, K.; Puett, D.; Tackett, R.L. Gender Differences in the Expression of Endothelin Receptors in Human Saphenous Veins in Vitro. J. Pharmacol. Exp. Ther. 1998, 285, 511–517. [Google Scholar] [PubMed]
- Tatchum-Talom, R.; Martel, C.; Labrie, C.; Labrie, F.; Marette, A. Gender Differences in Hemodynamic Responses to Endothelin-1. J. Cardiovasc. Pharmacol. 2000, 36, S102–S104. [Google Scholar] [CrossRef] [PubMed]
- Juan, S.; Chen, J.; Chen, C.; Lin, H.; Cheng, C.; Liu, J.; Hsieh, M.; Chen, Y.; Chao, H.; Chen, T. 17β-Estradiol Inhibits Cyclic Strain-Induced Endothelin-1 Gene Expression within Vascular Endothelial Cells. Am. J. Physiol. 2004, 287, H1254–H1261. [Google Scholar] [CrossRef] [PubMed]
- Axelsen, L.N.; Calloe, K.; Holstein-Rathlou, N.; Nielsen, M.S. Managing the Complexity of Communication: Regulation of Gap Junctions by Post-Translational Modification. Front. Pharmacol. 2013, 4, 130. [Google Scholar] [CrossRef] [PubMed]
- Van Kempen, M.J.; Jongsma, H.J. Distribution of connexin37, connexin40 and connexin43 in the Aorta and Coronary Artery of several Mammals. Histochem. Cell Biol. 1999, 112, 479–486. [Google Scholar]
- Hill, C.; Rummery, N.; Hickey, H.; Sandow, S.L. Heterogeneity in the Distribution of Vascular Gap Junctions and Connexins: Implications for Function. Clin. Exp. Pharmacol. Physiol. 2002, 29, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Yeh, H.I.; Rothery, S.; Dupont, E.; Coppen, S.R.; Severs, N.J. Individual Gap Junction Plaques Contain Multiple Connexins in Arterial Endothelium. Circ. Res. 1998, 83, 1248–1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaytor, A.T.; Bakker, L.M.; Edwards, D.H.; Griffith, T.M. Connexin-mimetic Peptides Dissociate Electrotonic EDHF-type Signalling Via Myoendothelial and Smooth Muscle Gap Junctions in the Rabbit Iliac Artery. Br. J. Pharmacol. 2005, 144, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Stauffer, B.L.; Sobus, R.D.; Sucharov, C.C. Sex Differences in Cardiomyocyte connexin43 Expression. J. Cardiovasc. Pharmacol. 2011, 58, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Di, W.; Lachelin, G.C.; McGarrigle, H.; Thomas, N.; Becker, D. Oestriol and Oestradiol Increase Cell to Cell Communication and connexin43 Protein Expression in Human Myometrium. Mol. Hum. Reprod. 2001, 7, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Dahl, G.; Werner, R. The connexin43 Gene is Responsive to Oestrogen. Proc. Biol. Sci. 1994, 255, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, S.; Kurihara, H.; Watanabe, M.; Okada, T.; Sakai, T.; Amano, A. Alterations of Phosphorylation State of Connexin 43 during Hypoxia and Reoxygenation are Associated with Cardiac Function. J. Histochem. Cytochem. 2006, 54, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Faigle, M.; Seessle, J.; Zug, S.; El Kasmi, K.C.; Eltzschig, H.K. ATP Release from Vascular Endothelia Occurs Across Cx43 Hemichannels and is Attenuated during Hypoxia. PLoS ONE 2008, 3, e2801. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Dai, D.; Dai, Y. CPU86017 and its Isomers Improve Hypoxic Pulmonary Hypertension by Attenuating Increased ETA Receptor Expression and Extracellular Matrix Accumulation. Naunyn Schmiedebergs Arch. Pharmacol. 2008, 378, 541. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Yin, N.; Hu, L.; Fan, H.; Yu, D.; Zhang, W.; Wang, S.; Feng, Y.; Fan, C.; Cao, F.; et al. Sildenefil Increases Connexin 40 in Smooth Muscle Cells through Activation of BMP Pathways in Pulmonary Arterial Hypertension. Int. J. Clin. Exp. Pathol. 2014, 7, 4674–4684. [Google Scholar] [PubMed]
- Schmidt, V.J.; Jobs, A.; von Maltzahn, J.; Wörsdörfer, P.; Willecke, K.; de Wit, C. Connexin45 is Expressed in Vascular Smooth Muscle but its Function Remains Elusive. PLoS ONE 2012, 7, e42287. [Google Scholar] [CrossRef] [PubMed]
- MacLean, M.R.; Deuchar, G.A.; Hicks, M.N.; Morecroft, I.; Shen, S.; Sheward, J.; Colston, J.; Loughlin, L.; Nilsen, M.; Dempsie, Y.; et al. Overexpression of the 5-Hydroxytryptamine Transporter Gene: Effect on Pulmonary Hemodynamics and Hypoxia-Induced Pulmonary Hypertension. Circulation 2004, 109, 2150–2155. [Google Scholar] [CrossRef] [PubMed]
- Dempsie, Y.; Nilsen, M.; White, K.; Mair, K.M.; Loughlin, L.; Ambartsumian, N.; Rabinovitch, M.; MacLean, M.R. Development of Pulmonary Arterial Hypertension in Mice Over-Expressing S100A4/Mts1 is Specific to Females. Respir. Res. 2011, 12, 159. [Google Scholar] [CrossRef] [PubMed]
- Dempsie, Y.; MacRitchie, N.A.; White, K.; Morecroft, I.; Wright, A.F.; Nilsen, M.; Loughlin, L.; Mair, K.M.; MacLean, M.R. Dexfenfluramine and the Oestrogen-Metabolizing Enzyme CYP1B1 in the Development of Pulmonary Arterial Hypertension. Cardiovasc. Res. 2013, 99, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Michela, P.; Velia, V.; Aldo, P.; Ada, P. Role of Connexin 43 in Cardiovascular Diseases. Eur. J. Pharmacol. 2015, 768, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Isakson, B.E.; Damon, D.N.; Day, K.H.; Liao, Y.; Duling, B.R. Connexin40 and connexin43 in Mouse Aortic Endothelium: Evidence for Coordinated Regulation. Am J. Physiol. 2006, 290, H1199–H1205. [Google Scholar] [CrossRef] [PubMed]
- Kruger, O.; Beny, J.L.; Chabaud, F.; Traub, O.; Theis, M.; Brix, K.; Kirchhoff, S.; Willecke, K. Altered Dye Diffusion and Upregulation of connexin37 in Mouse Aortic Endothelium Deficient in connexin40. J. Vasc. Res. 2002, 39, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Simon, A.M.; McWhorter, A.R. Decreased Intercellular Dye-Transfer and Downregulation of Non-Ablated Connexins in Aortic Endothelium Deficient in connexin37 or connexin40. J. Cell Sci. 2003, 116, 2223–2236. [Google Scholar] [CrossRef] [PubMed]
- Giaid, A.; Saleh, D. Reduced Expression of Endothelial Nitric Oxide Synthase in the Lungs of Patients with Pulmonary Hypertension. N. Engl. J. Med. 1995, 333, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.Y.; Zhao, Y.D.; Mirza, M.K.; Huang, J.H.; Potula, H.H.; Vogel, S.M.; Brovkovych, V.; Yuan, J.X.; Wharton, J.; Malik, A.B. Persistent eNOS Activation Secondary to Caveolin-1 Deficiency Induces Pulmonary Hypertension in Mice and Humans through PKG Nitration. J. Clin. Investig. 2009, 119, 2009–2018. [Google Scholar] [CrossRef] [PubMed]
- Mason, N.A.; Springall, D.R.; Burke, M.; Pollock, J.; Mikhail, G.; Yacoub, M.H.; Polak, J.M. High Expression of Endothelial Nitric Oxide Synthase in Plexiform Lesions of Pulmonary Hypertension. J. Pathol. 1998, 185, 313–318. [Google Scholar] [CrossRef]
- Kaneko, F.T.; Arroliga, A.C.; Dweik, R.A.; Comhair, S.A.; Laskowski, D.; Oppedisano, R.; Thomassen, M.J.; Erzurum, S.C. Biochemical Reaction Products of Nitric Oxide as Quantitative Markers of Primary Pulmonary Hypertension. Am. J. Respir. Crit. Care Med. 1998, 158, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.D.; Hamid, R.; Hemnes, A.R.; Loyd, J.E.; Blackwell, T.; Yu, C.; Phillips III, J.A.; Gaddipati, R.; Gladson, S.; Gu, E. BMPR2 Expression is Suppressed by Signaling through the Estrogen Receptor. Biol. Sex Differ. 2012, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Keegan, A.; Morecroft, I.; Smillie, D.; Hicks, M.N.; MacLean, M.R. Contribution of the 5-HT(1B) Receptor to Hypoxia-Induced Pulmonary Hypertension: Converging Evidence using 5-HT(1B)-Receptor Knockout Mice and the 5-HT(1B/1D)-Receptor Antagonist GR127935. Circ. Res. 2001, 89, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Morecroft, I.; Pang, L.; Baranowska, M.; Nilsen, M.; Loughlin, L.; Dempsie, Y.; Millet, C.; MacLean, M.R. In Vivo Effects of a Combined 5-HT1B receptor/SERT Antagonist in Experimental Pulmonary Hypertension. Cardiovasc. Res. 2009, 85, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Chaytor, A.T.; Evans, W.H.; Griffith, T.; Thornbury, K. Peptides Homologous to Extracellular Loop Motifs of Connexin 43 Reversibly Abolish Rhythmic Contractile Activity in Rabbit Arteries. J. Physiol. 1997, 503, 99–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glass, B.J.; Hu, R.G.; Phillips, A.R.; Becker, D.L. The Action of Mimetic Peptides on Connexins Protects Fibroblasts from the Negative Effects of Ischemia Reperfusion. Biol. Open 2015, 4, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Faniku, C.; O’Shaughnessy, E.; Lorraine, C.; Johnstone, S.R.; Graham, A.; Greenhough, S.; Martin, P.E. The Connexin Mimetic Peptide Gap27 and Cx43-Knockdown Reveal Differential Roles for Connexin43 in Wound Closure Events in Skin Model Systems. Int. J. Mol. Sci. 2018, 19, 604. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.S.; Pollok, S.; Flint, D.J.; Brandner, J.M.; Martin, P.E. The Connexin Mimetic Peptide Gap27 Increases Human Dermal Fibroblast Migration in Hyperglycemic and Hyperinsulinemic Conditions in Vitro. J. Cell. Physiol. 2012, 227, 77–87. [Google Scholar] [CrossRef] [PubMed]









| Agonists | Groups | Log EC50 (M) | Emax (%) | Global Shift in Concentration Response Curve | n |
|---|---|---|---|---|---|
| ET-1 | Male WT | −8.46 ± 0.08 | 131.8 ± 2.5 | NS | 6 |
| Male Cx43+/− | −8.77 ± 0.12 * | 127.4 ± 2.8 | 5 | ||
| ET-1 | Female WT | −8.31 ± 0.06 | 126 ± 2.2 | NS | 5 |
| Female Cx43+/− | −8.48 ± 0.04 | 130.3 ± 4.5 | 7 | ||
| 5-HT | Male WT | −6.67 ± 0.05 | 112.7 ± 2.8 | NS | 6 |
| Male Cx43+/− | −6.64 ± 0.07 | 118.9 ± 4.8 | 5 | ||
| 5-HT | Female WT | −6.82 ± 0.05 | 119.6 ± 3.5 | NS | 5 |
| Female Cx43+/− | −6.83 ± 0.1 | 116.6 ± 6.7 | 5 |
| Agonists | Groups | Log EC50 (M) | Rmax (%) | Global Shift in Concentration Response Curve | n |
|---|---|---|---|---|---|
| MCh | Male WT | −6.93 ± 0.08 | 55.6 ± 6.8 | **** | 5 |
| Male Cx43+/− | −7.14 ± 0.21 ** | 28 ± 4.1 ** | 5 | ||
| MCh | Female WT | −6.52 ± 0.14 | 55.3 ± 8.5 | **** | 6 |
| Female Cx43+/− | −6.48 ± 0.24 | 26.8 ± 7.8 * | 6 | ||
| MCh | Male WT | −6.39 ± 0.2 | 42.1 ± 4.6 | **** | 6 |
| Plus 37,43Gap27 | −6.08 ± 0.1 **** | 22.9 ± 5.6 * | 6 | ||
| MCh | Female WT | −6.8 ± 0.08 | 63.1 ± 4.8 | **** | 6 |
| Plus 37,43Gap27 | −6.36 ± 0.1 ** | 42.2 ± 5.2 * | 6 | ||
| MCh | Male WT | −6.27 ± 0.11 | 32.8 ± 4.6 | **** | 6 |
| Plus l-NAME | not applicable | 2.2 ± 3.4 *** | 6 | ||
| Isoprenaline | Male WT | −7.77 ± 0.17 | 92.1 ± 1.19 | **** | 5 |
| Plus 37,43Gap27 | −7.41 ± 0.16 | 80.8 ± 4.2 * | 5 | ||
| Isoprenaline | Male WT | −7.84 ± 0.2 | 86.7 ± 3.2 | **** | 6 |
| Plus l-NAME | −7.5 ± 0.13 | 60.4 ± 4.3 *** | 6 |
| Agonists | Genotypes | Log EC50 (M) | Emax (%) | Global Shift in Concentration Response Curve | n |
|---|---|---|---|---|---|
| ET-1 | Hypoxic WT | −7.95 ± 0.06 | 91.7 ± 8.1 | ** | 6 |
| Hypoxic Cx43+/− | −8.07 ± 0.09 *** | 112.7 ± 5.6 * | 7 | ||
| 5-HT | Hypoxic WT | −6.56 ± 0.04 | 126 ± 2.2 | NS | 7 |
| Hypoxic Cx43+/− | −6.5 ± 0.03 | 130.3 ± 4.5 | 7 |
| Gene | Sequence | Product Length (Base Pairs) | Tm (°C) |
|---|---|---|---|
| GJA1 (Cx43) | Sense-ACTGAGCCCATCCAAAGACT Antisense-CAGGAGGAGACATAGGTGAGAG | 95 | Sense-56.6 Antisense-57.3 |
| GJA5 (Cx40) | Sense-ATGGTATACTCTCCTCAGCACTAC Antisense-CCAGTCATTGAGAAGACTCAGAAC | 117 | Sense-56.8 Antisense-57 |
| GJA4 (Cx37) | Sense-ACACCCACCCTGATCTACCT Antisense-TCCCTCTTTCTGCCGCAAC | 75 | Sense-57.5 Antisense-58 |
| GJC1 (Cx45) | Sense-CAGAGATGGAGTTAGAAAGCGAAA Antisense-AAGCCCACCTCAAACACAGT | 148 | Sense-57.8 Antisense-57.7 |
| Panx1 | Sense-TCAGCCTCATTAACCTCATTGTG Antisense-TGGGCAGGATTTCATACACTTTG | 114 | Sense-57.5 Antisense-58 |
| NOS3 (eNOS) | Sense-GGAAGTAGCCAATGCAGTGAA Antisense-GCCAGTCTCAGAGCCATACA | 97 | Sense-56.8 Antisense-57.2 |
| BMPR2 (BMPRII) | Sense-TGTTATCAGTGACTTTGGTTTATCC Antisense-CTTATAGCCCGCATTATCTTCTTCC | 84 | Sense-56.5 Antisense-56.3 |
| Tph1 | Sense-AATTCACGGAAGAAGAGATTAAGAC Antisense-CCAGTTGCGGGATGTTGTC | 150 | Sense-56.3 Antisense-56.9 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Htet, M.; Nally, J.E.; Shaw, A.; Foote, B.E.; Martin, P.E.; Dempsie, Y. Connexin 43 Plays a Role in Pulmonary Vascular Reactivity in Mice. Int. J. Mol. Sci. 2018, 19, 1891. https://doi.org/10.3390/ijms19071891
Htet M, Nally JE, Shaw A, Foote BE, Martin PE, Dempsie Y. Connexin 43 Plays a Role in Pulmonary Vascular Reactivity in Mice. International Journal of Molecular Sciences. 2018; 19(7):1891. https://doi.org/10.3390/ijms19071891
Chicago/Turabian StyleHtet, Myo, Jane E. Nally, Andrew Shaw, Bradley E. Foote, Patricia E. Martin, and Yvonne Dempsie. 2018. "Connexin 43 Plays a Role in Pulmonary Vascular Reactivity in Mice" International Journal of Molecular Sciences 19, no. 7: 1891. https://doi.org/10.3390/ijms19071891