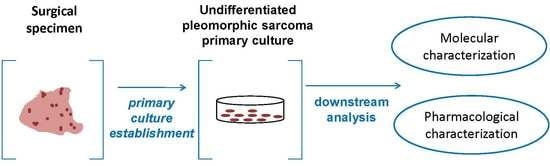
Primary Culture of Undifferentiated Pleomorphic Sarcoma: Molecular Characterization and Response to Anticancer Agents
Abstract
:1. Introduction
2. Results
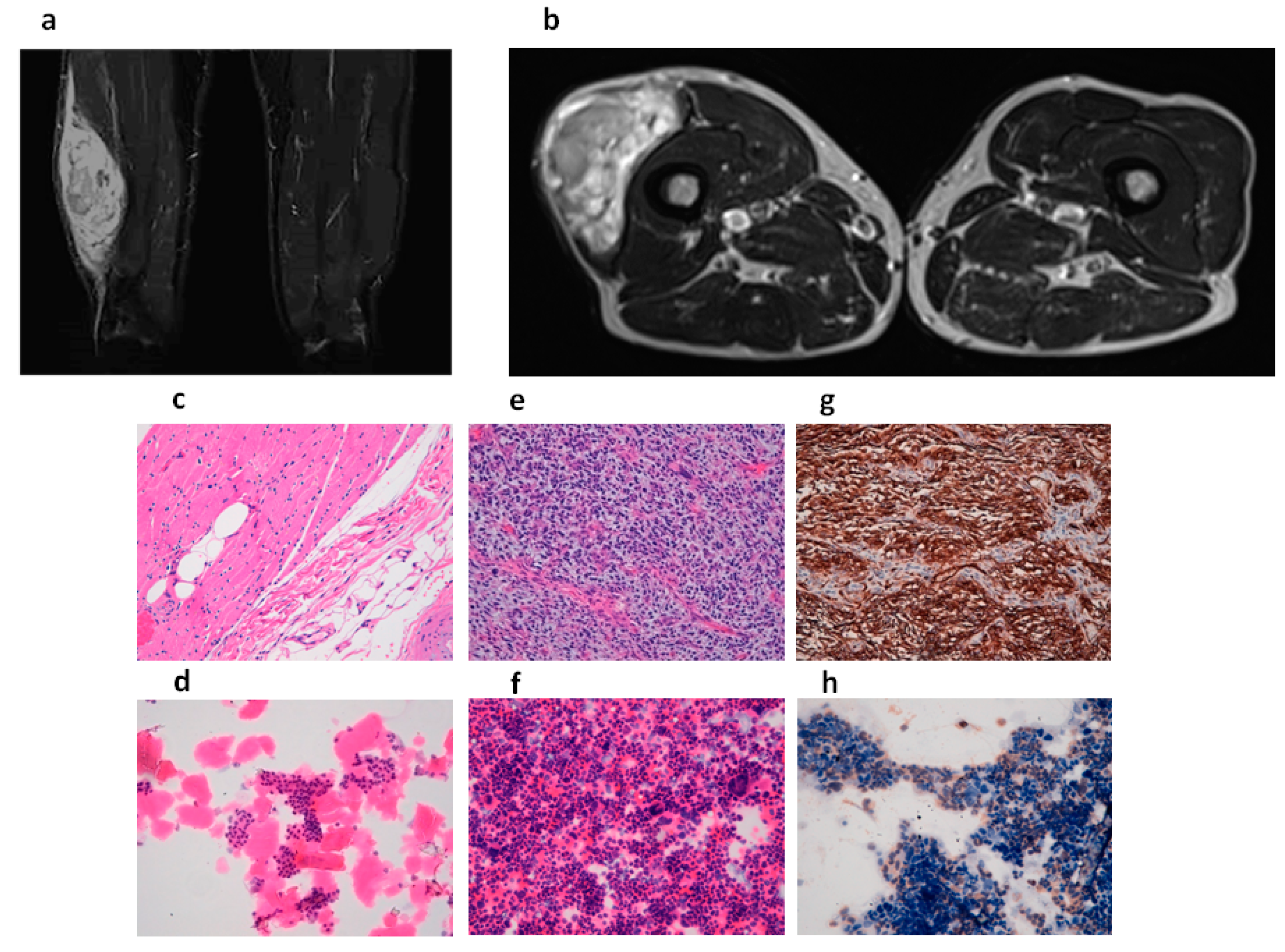
2.1. Tumor Diagnosis
2.2. Establishment of Patient-Derived Undifferentiated Pleomorphic Sarcoma (UPS) Culture
2.3. Gene Expression Profile of Patient-Derived UPS Culture
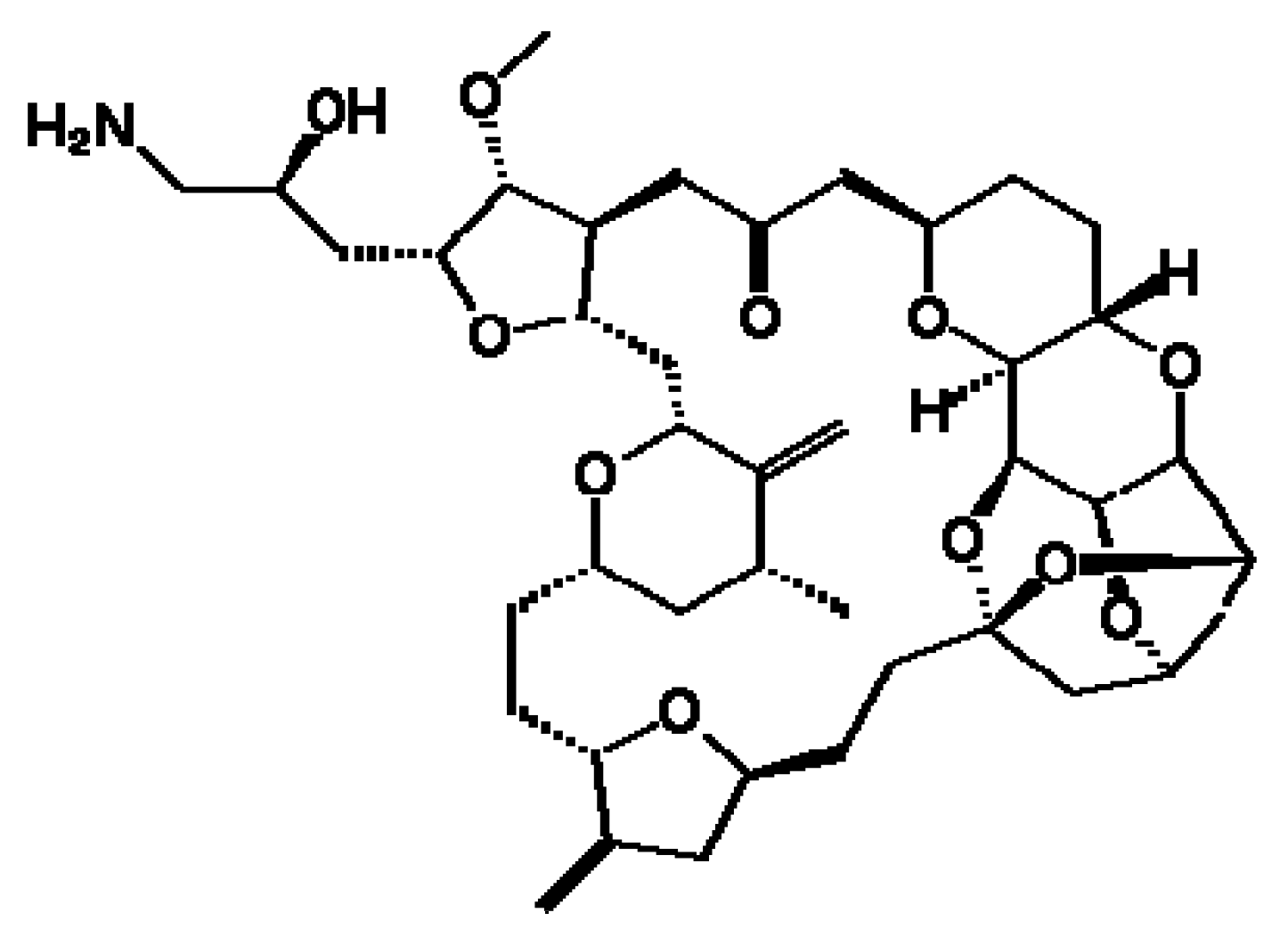
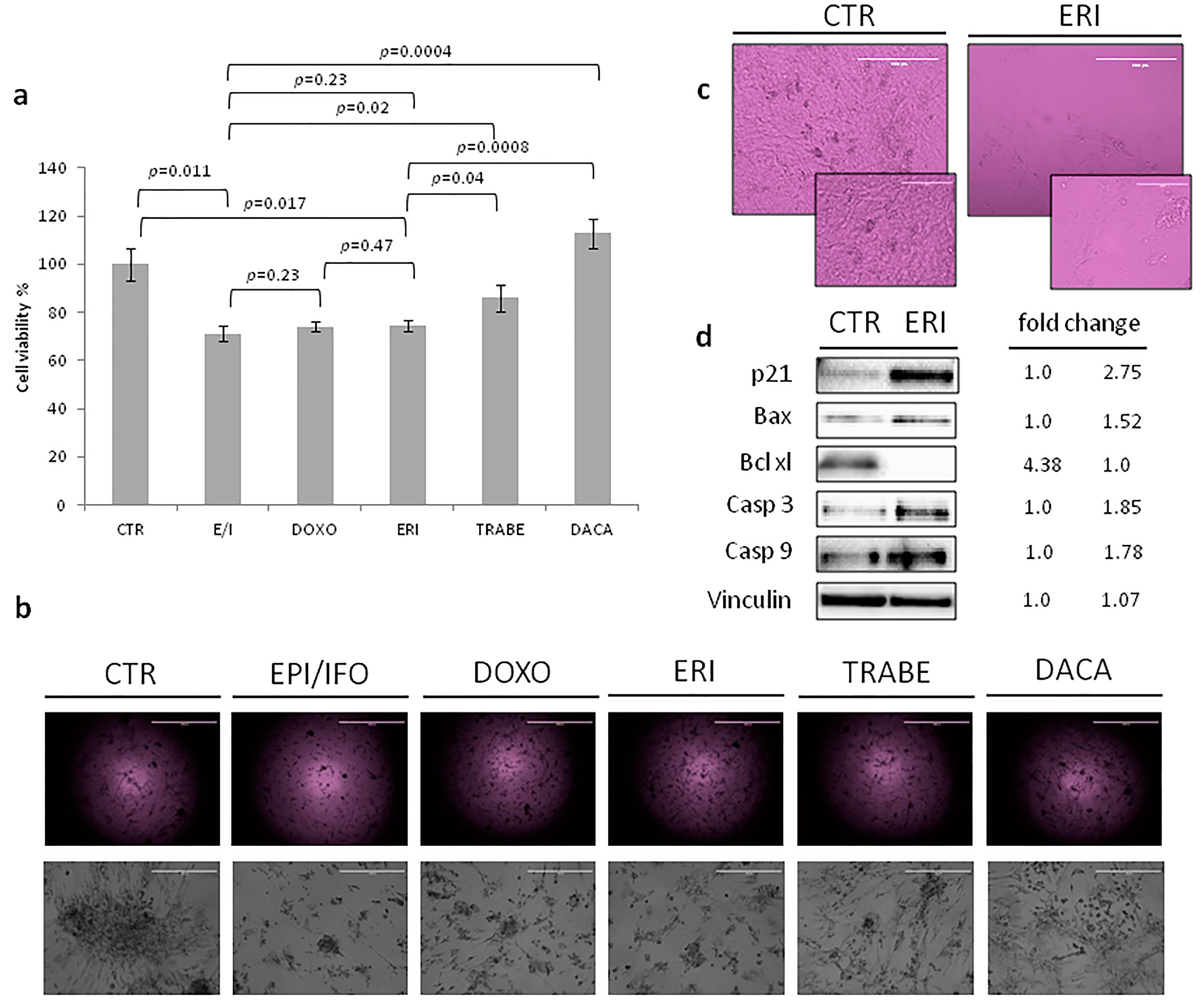
2.4. Chemotherapy Assessment in UPS Primary Culture
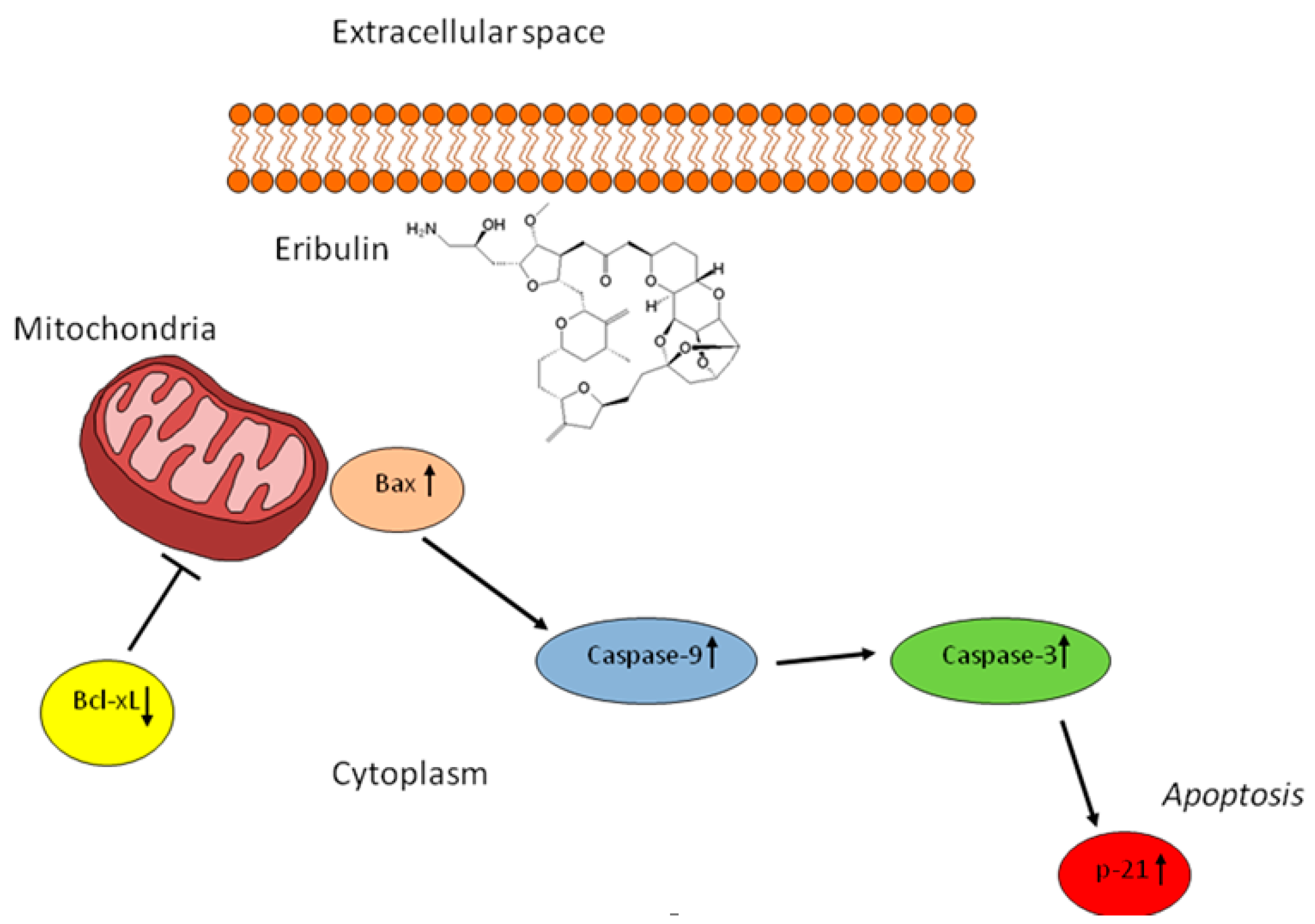
2.5. The Activity of Eribulin in the UPS Primary Culture
3. Discussion
4. Experimental Section
4.1. Ethics Statement
4.2. Patient History
4.3. Histological and Immunohistochemical Diagnosis
4.4. Establishment of UPS Primary Cell Culture
4.5. Histological and Immunohistochemical Analysis of UPS Primary Culture
4.6. Gene Expression Analysis
4.7. Drug Testing
4.8. Protein Expression Analysis
4.9. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fletcher, C.D.M.; Bridge, J.A.; Hogendoorn, P.; Mertens, F. WHO Classification of Tumours of Soft Tissue Sarcoma and Bone, 4th ed.; IARC Press: Lyon, France, 2013; pp. 236–237. ISBN 13 9789283224341. [Google Scholar]
- Alaggio, R.; Collini, P.; Randall, R.L.; Barnette, P.; Million, L.; Coffin, C.M. Undifferentiated high-grade pleomorphic sarcomas in children: A clinicopathologic study of 10 cases and review of literature. Pediatr. Dev. Pathol. 2010, 13, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Goldblum, J.R. An approach to pleomorphic sarcomas: Can we subclassify, and does it matter? Mod. Pathol. 2014, 27, S39–S46. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, A.F.; Raut, C.P. Diagnosis and management of pleomorphic sarcomas (so-called “MFH”) in adults. J. Surg. Oncol. 2008, 97, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Saponara, M.; Stacchiotti, S.; Casali, P.G.; Gronchi, A. (Neo)adjuvant treatment in localised soft tissue sarcoma: The unsolved affair. Eur. J. Cancer 2017, 70, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, D.P.; Rushing, C.N.; Lane, W.O.; Cardona, D.M.; Kirsch, D.G.; Peterson, B.L.; Blazer, D.G., 3rd. Preoperative or postoperative radiotherapy versus surgery alone for retroperitoneal sarcoma: A case-control, propensity score-matched analysis of a nationwide clinical oncology database. Lancet Oncol. 2016, 17, 966–975. [Google Scholar] [CrossRef]
- McBride, S.M.; Raut, C.P.; Lapidus, M.; Devlin, P.M.; Marcus, K.J.; Bertagnolli, M.; George, S.; Baldini, E.H. Locoregional recurrence after preoperative radiation therapy for retroperitoneal sarcoma: Adverse impact of multifocal disease and potential implications of dose escalation. Ann. Surg. Oncol. 2013, 20, 2140–2147. [Google Scholar] [CrossRef] [PubMed]
- Kearney, M.M.; Soule, E.H.; Ivins, J.C. Malignant fibrous histiocytoma: A retrospective study of 167 cases. Cancer 1980, 45, 167–178. [Google Scholar] [CrossRef]
- Pezzi, C.M.; Rawlings, M.S., Jr.; Esgro, J.J.; Pollock, R.E.; Romsdahl, M.M. Prognostic factors in 227 patients with malignant fibrous histiocytoma. Cancer 1992, 69, 2098–2103. [Google Scholar] [CrossRef]
- Schoenfeld, D.; Rosenbaum, C.; Horton, J. A comparison of Adriamycin versus vincristine and Adriamycin and cyclophosphamide for advanced sarcoma. Cancer 1982, 50, 2757–2762. [Google Scholar] [CrossRef]
- Bramwell, V.H.C.; Anderson, D.; Charette, M.L. Doxorubicin-based chemotherapy for the palliative treatment of adult patients with locally advanced or metastatic soft-tissue sarcoma: A meta-analysis and clinical practice guideline. Sarcoma 2000, 4, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Judson, I.; Verweij, J.; Gelderblom, H.; Hartmann, J.T.; Schöffski, P.; Blay, J.Y.; Kerst, J.M.; Sufliarsky, J.; Whelan, J.; Hohenberger, P.; et al. Doxorubicin alone versus intensified doxorubicin plus ifosfamide for first-line treatment of advanced or metastatic soft-tissue sarcoma: A randomised controlled phase 3 trial. Lancet Oncol. 2014, 15, 415–423. [Google Scholar] [CrossRef]
- Gronchi, A.; Stacchiotti, S.; Verderio, P.; Ferrari, S.; Martin Broto, J.; Lopez-Pousa, A.; Llombart-Bosch, A.; Dei Tos, A.P.; Collini, P.; Jurado, J.C.; et al. Short, full-dose adjuvant chemotherapy (CT) in high-risk adult soft tissue sarcomas (STS): Long-term follow-up of a randomized clinical trial from the Italian Sarcoma Group and the Spanish Sarcoma Group. Ann. Oncol. 2016, 27, 2283–2288. [Google Scholar] [CrossRef] [PubMed]
- Swami, U.; Shah, U.; Goel, S. Eribulin in cancer treatment. Mar. Drugs 2015, 13, 5016–5058. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Movva, S. Eribulin in the management of inoperable soft-tissue sarcoma: Patient selection and survival. Onco Targets Ther. 2016, 9, 5619–5627. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A.; Wilson, L.; Azarenko, O.; Zhu, X.; Lewis, B.M.; Littlefield, B.A.; Jordan, M.A. Eribulin binds at microtubule ends to a single site on tubulin to suppress dynamic instability. Biochemistry 2010, 49, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Jordan, M.A.; Kamath, K.; Manna, T.; Okouneva, T.; Miller, H.P.; Davis, C.; Littlefield, B.A.; Wilson, L. The primary antimitotic mechanism of action of the synthetic halichondrin E7389 is suppression of microtubule growth. Mol. Cancer Ther. 2005, 4, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsov, G.; Towle, M.J.; Cheng, H.; Kawamura, T.; TenDyke, K.; Liu, D.; Kishi, Y.; Yu, M.J.; Littlefield, B.A. Induction of morphological and biochemical apoptosis following prolonged mitotic blockage by halichondrin B macrocyclic ketone analog E7389. Cancer Res. 2004, 64, 5760–5766. [Google Scholar] [CrossRef] [PubMed]
- Towle, M.J.; Salvato, K.A.; Budrow, J.; Wels, B.F.; Kuznetsov, G.; Aalfs, K.K.; Welsh, S.; Zheng, W.; Seletsky, B.M.; Palme, M.H.; et al. In vitro and in vivo anticancer activities of synthetic macrocyclic ketone analogues of halichondrin B. Cancer Res. 2001, 61, 1013–1021. [Google Scholar] [PubMed]
- Funahashi, Y.; Okamoto, K.; Adachi, Y.; Semba, T.; Uesugi, M.; Ozawa, Y.; Tohyama, O.; Uehara, T.; Kimura, T.; Watanabe, H.; et al. Eribulin mesylate reduces tumor microenvironment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci. 2014, 105, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Hirata, Y.; Suzuki, N.; Ihara, S.; Sakitani, K.; Kobayashi, Y.; Kinoshita, H.; Hayakawa, Y.; Yamada, A.; Watabe, H.; et al. Characterization of a new small bowel adenocarcinoma cell line and screening of anti-cancer drug against small bowel adenocarcinoma. Am. J. Pathol. 2015, 185, 550–562. [Google Scholar] [CrossRef] [PubMed]
- De Vita, A.; Miserocchi, G.; Recine, F.; Mercatali, L.; Pieri, F.; Medri, L.; Bongiovanni, A.; Cavaliere, D.; Liverani, C.; Spadazzi, C.; et al. Activity of eribulin in a primary culture of well-differentiated/dedifferentiated adipocytic sarcoma. Molecules 2016, 21, 1662. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Ozawa, Y.; Kimura, T.; Sato, Y.; Kuznetsov, G.; Xu, S.; Uesugi, M.; Agoulnik, S.; Taylor, N.; Funahashi, Y.; et al. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br. J. Cancer 2014, 110, 1497–1505. [Google Scholar] [CrossRef] [PubMed]
- Schöffski, P.; Ray-Coquard, I.L.; Cioffi, A.; Bui, N.B.; Bauer, S.; Hartmann, J.T.; Krarup-Hansen, A.; Grünwald, V.; Sciot, R.; Dumez, H.; et al. Activity of eribulin mesylate in patients with soft-tissue sarcoma: A phase 2 study in four independent histological subtypes. Lancet Oncol. 2011, 12, 1045–1052. [Google Scholar] [CrossRef]
- Schöffski, P.; Chawla, S.; Maki, R.G.; Italiano, A.; Gelderblom, H.; Choy, E.; Grignani, G.; Camargo, V.; Bauer, S.; Rha, S.Y.; et al. Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: A randomised, open-label, multicentre, phase 3 trial. Lancet 2016, 387, 1629–1637. [Google Scholar] [CrossRef]
- Kawai, A.; Araki, N.; Naito, Y.; Ozaki, T.; Sugiura, H.; Yazawa, Y.; Morioka, H.; Matsumine, A.; Saito, K.; Asami, S.; et al. Phase 2 study of eribulin in patients with previously treated advanced or metastatic soft tissue sarcoma. Jpn. J. Clin. Oncol. 2017, 47, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Emambux, S.; Kind, M.; Le Loarer, F.; Toulmonde, M.; Stoeckle, E.; Italiano, A. Clinical activity of eribulin in advanced desmoplastic small round-cell tumor. Anticancer Drugs 2017, 28, 1053–1055. [Google Scholar] [CrossRef] [PubMed]
- Nishio, J.; Iwasaki, H.; Ishiguro, M.; Ohjimi, Y.; Nishimura, N.; Koga, T.; Kawarabayashi, T.; Kaneko, Y.; Kikuchi, M. Establishment of a new human malignant fibrous histiocytoma cell line, FU-MFH-1: Cytogenetic characterization by comparative genomic hybridization and fluorescence in situ hybridization. Cancer Genet. Cytogenet. 2003, 144, 44–51. [Google Scholar] [CrossRef]
- Pan, X.; Yoshida, A.; Kawai, A.; Kondo, T. Current status of publicly available sarcoma cell lines for use in proteomic studies. Expert Rev. Proteom. 2016, 13, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Demetri, G.D.; von Mehren, M.; Jones, R.L.; Jones, R.L.; Hensley, M.L.; Schuetze, S.M.; Staddon, A.; Milhem, M.; Elias, A.; Ganjoo, K.; et al. Efficacy and safety of trabectedin or dacarbazine for metastatic liposarcoma or leiomyosarcoma after failure of conventional chemotherapy: Results of a phase III randomized multicenter clinical trial. J. Clin. Oncol. 2016, 34, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Demetri, G.D.; Chawla, S.P.; von Mehren, M.; Ritch, P.; Baker, L.H.; Blay, J.Y.; Hande, K.R.; Keohan, M.L.; Samuels, B.L.; Schuetze, S.; et al. Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: Results of a randomized phase II study of two different schedules. J. Clin. Oncol. 2009, 27, 4188–4196. [Google Scholar] [CrossRef] [PubMed]
- Recine, F.; Bongiovanni, A.; Riva, N.; Fausti, V.; De Vita, A.; Mercatali, L.; Liverani, C.; Miserocchi, G.; Amadori, D.; Ibrahim, T. Update on the role of trabectedin in the treatment of intractable soft tissue sarcomas. Onco Targets Ther. 2017, 10, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Weaver, J.; Downs-Kelly, E.; Goldblum, J.R.; Turner, S.; Kulkarni, S.; Tubbs, R.R.; Rubin, B.P.; Skacel, M. Fluorescence in situ hybridization for MDM2 gene amplification as a diagnostic tool in lipomatous neoplasms. Mod. Pathol. 2008, 21, 943–949. [Google Scholar] [CrossRef] [PubMed]
- De Vita, A.; Mercatali, L.; Recine, F.; Pieri, F.; Riva, N.; Bongiovanni, A.; Liverani, C.; Spadazzi, C.; Miserocchi, G.; Amadori, D.; et al. Current classification, treatment options, and new perspectives in the management of adipocytic sarcomas. Onco Targets Ther. 2016, 9, 6233–6246. [Google Scholar] [CrossRef] [PubMed]
- Hogue, D.L.; Nash, C.; Ling, V.; Hobman, T.C. Lysosome-associated protein transmembrane 4 alpha (LAPTM4 alpha) requires two tandemly arranged tyrosine-based signals for sorting to lysosomes. Biochem. J. 2002, 365, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zou, L.; Li, Q.; Haibe-Kains, B.; Tian, R.; Li, Y.; Desmedt, C.; Sotiriou, C.; Szallasi, Z.; Iglehart, J.D.; et al. Amplification of LAPTM4B and YWHAZ contributes to chemotherapy resistance and recurrence of breast cancer. Nat. Med. 2010, 16, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Ozzello, L.; Stout, A.P.; Murray, M.R. Cultural characteristics of malignant histiocytomas and fibrous xanthomas. Cancer 1963, 16, 331–334. [Google Scholar] [CrossRef]
- O’Brien, J.E.; Stout, A.P. Malignant fibrous xanthomas. Cancer 1964, 17, 1445–1455. [Google Scholar] [CrossRef]
- Montgomery, E.; Fisher, C. Myofibroblastic differentiation in malignant fibrous histiocytoma (pleomorphic myofibrosarcoma): A clinicopathological study. Histopathology 2001, 38, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Weiss, S.W.; Enzinger, F.M. Malignant fibrous histiocytoma: An analysis of 200 cases. Cancer 1978, 41, 2250–2266. [Google Scholar] [CrossRef]
- Belal, A.; Kandil, A.; Allam, A.; Khafaga, Y.; El-Husseiny, G.; El-Enbaby, A.; Memon, M.; Younge, D.; Moreau, P.; Gray, A.; et al. Malignant fibrous histiocytoma: A retrospective study of 109 cases. Am. J. Clin. Oncol. 2002, 25, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Adrianzen Herrera, D.A.; Kuk, D.; Keohan, M.L.; Dickson, M.A.; D’Angelo, S.P.; Ping, C.; Agaram, N.P.; Antonescu, C.R.; Hameed, M.; Tap, W.D.; et al. Outcomes of systemic therapy for patients with metastatic undifferentiated pleomorphic sarcoma (UPS). J. Clin. Oncol. 2016, 34, 11066. [Google Scholar] [CrossRef]
- Miserocchi, G.; Mercatali, L.; Liverani, C.; De Vita, A.; Spadazzi, C.; Pieri, F.; Bongiovanni, A.; Recine, F.; Amadori, D.; Ibrahim, T. Management and potentialities of primary cancer cultures in preclinical and translational studies. J. Transl. Med. 2017, 15, 229. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, K.; Kawaguchi, K.; Kiyuna, T.; Murakami, T.; Miwa, S.; Nelson, S.D.; Dry, S.M.; Li, Y.; Singh, A.S.; Kimura, H.; et al. Efficacy in vitro of caffeine and valproic acid on patient-derived undifferentiated pleomorphic sarcoma and rhabdomyosarcoma cell lines. Anticancer Res. 2017, 37, 4081–4084. [Google Scholar] [CrossRef] [PubMed]
- Salawu, A.; Fernando, M.; Hughes, D.; Reed, M.W.; Woll, P.; Greaves, C.; Day, C.; Alhajimohammed, M.; Sisley, K. Establishment and molecular characterization of seven novel soft-tissue sarcoma cell lines. Br. J. Cancer 2016, 115, 1058–1068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlott, T.; Taubert, H.; Fayyazi, A.; Schweyer, S.; Bartel, F.; Korabiowska, M.; Brinck, U. Analysis of central regulatory pathways in p53-deficient primary cultures of malignant fibrous histiocytoma exposed to ifosfamide. Anticancer Res. 2004, 24, 3819–3829. [Google Scholar] [PubMed]
- Igarashi, K.; Kawaguchi, K.; Murakami, T.; Kiyuna, T.; Miyake, K.; Yamamoto, N.; Hayashi, K.; Kimura, H.; Nelson, S.D.; Dry, S.M.; et al. A novel anionic-phosphate-platinum complex effectively targets an undifferentiated pleomorphic sarcoma better than cisplatinum and doxorubicin in a patient-derived orthotopic xenograft (PDOX). Oncotarget 2017, 8, 63353–63359. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; He, X.D.; Yu, J.C.; Zhou, R.L.; Shan, Y.; Rui, J.A. Overexpression of LAPTM4B-35 attenuates epirubucin induced apoptosis of gallbladder carcinoma GBC-SD cells. Surgery 2011, 150, 25–31. [Google Scholar] [CrossRef] [PubMed]
- De Vita, A.; Recine, F.; Mercatali, L.; Miserocchi, G.; Liverani, L.; Spadazzi, L.; Casadei, R.; Bongiovanni, A.; Pieri, F.; Riva, N.; et al. Myxofibrosarcoma primary cultures: Molecular and pharmacological profile. Ther. Adv. Med. Oncol. 2017, in press. [Google Scholar] [CrossRef]
- Emori, M.; Tsukahara, T.; Murata, K.; Sugita, S.; Sonoda, T.; Kaya, M.; Soma, T.; Sasaki, M.; Nagoya, S.; Hasegawa, T.; et al. Prognostic impact of CD109 expression in myxofibrosarcoma. J. Surg. Oncol. 2015, 111, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, J.; Ouali, M.; Chaltiel, L.; Le Guellec, S.; Le Cesne, A.; Blay, J.Y.; Cousin, P.; Chaigneau, L.; Bompas, E.; Piperno-Neumann, S.; et al. Efficacy of trabectedin in malignant solitary fibrous tumors: A retrospective analysis from the French Sarcoma Group. BMC Cancer 2015, 15, 700. [Google Scholar] [CrossRef] [PubMed]
- Le Cesne, A.; Cresta, S.; Maki, R.G.; Blay, J.Y.; Verweij, J.; Poveda, A.; Casali, P.G.; Balaña, C.; Schöffski, P.; Grosso, F.; et al. A retrospective analysis of antitumour activity with trabectedin in translocation-related sarcomas. Eur. J. Cancer 2012, 48, 3036–3044. [Google Scholar] [CrossRef] [PubMed]
- Sabattini, E.; Bisgaard, K.; Ascani, S.; Poggi, S.; Piccioli, M.; Ceccarelli, C.; Pieri, F.; Fraternali-Orcioni, G.; Pileri, S.A. Envision Plus: A new immunohistochemical method of choice for diagnostics and research. Critical comparison with the APAAP, ChemMate CSA, LABC, and SABC techniques. J. Clin. Pathol. 1998, 51, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Highley, M.S.; Momerency, G.; Sawyers, D.; de Bruijn, E.A.; Prenen, H.; Guetens, G.; de Boeck, G.; van Oosterom, A.T.; Mansi, J.L.; Blake, P.R.; et al. The neurotoxicity and pharmacokinetics of oral ifosfamide. J. Anal. Oncol. 2015, 4, 13–23. [Google Scholar] [CrossRef]
- Cerny, T.; Leyvraz, S.; von Briel, T.; Küpfer, A.; Schaad, R.; Schmitz, S.F.; Honegger, P.; Sessa, C.; Brunner, J.; Boddy, A.V. Saturable metabolism of continuous high-dose ifosfamide with mesna and GM-CSF: A pharmacokinetic study in advanced sarcoma patients. Swiss Group for Clinical Cancer Research (SAKK). Ann. Oncol. 1999, 10, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Fogli, S.; Danesi, R.; Gennari, A.; Donati, S.; Conte, P.F.; del Tacca, M. Gemcitabine, epirubicin and paclitaxel: Pharmacokinetic and pharmacodynamic interactions in advanced breast cancer. Ann. Oncol. 2002, 13, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Robert, J.; Vrignaud, P.; Nguyen-Ngoc, T.; Iliadis, A.; Mauriac, L.; Hurteloup, P. Comparative pharmacokinetics and metabolism of doxorubicin and epirubicin in patients with metastatic breast cancer. Cancer Treat. Rep. 1985, 69, 633–640. [Google Scholar] [PubMed]
- Danesi, R.; Innocenti, F.; Fogli, S.; Gennari, A.; Baldini, E.; di Paolo, A.; Salvadori, B.; Bocci, G.; Conte, P.F.; Del Tacca, M. Pharmacokinetics and pharmacodynamics of combination chemotherapy with paclitaxel and epirubicinin breast cancer patients. Br. J. Clin. Pharmacol. 2002, 53, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Devriese, L.A.; Witteveen, P.E.; Wanders, J.; Law, K.; Edwards, G.; Reyderman, L.; Copalu, W.; Peng, F.; Marchetti, S.; Beijnen, J.H.; et al. Pharmacokinetics of eribulin mesylate in patients with solid tumours receiving repeated oral rifampicin. Br. J. Clin. Pharmacol. 2013, 75, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Van Kesteren, C.H.; de Vooght, M.M.; López-Lázaro, L.; Mathôt, R.A.; Schellens, J.H.; Jimeno, J.M.; Beijnen, J.H. Yondelis (trabectedin, ET-743): The development of an anticancer agent of marine origin. Anticancer Drugs 2003, 14, 487–502. [Google Scholar] [CrossRef] [PubMed]
- Brendel, E.; Ludwig, M.; Lathia, C.; Robert, C.; Ropert, S.; Soria, J.C.; Armand, J.P. Pharmacokinetic results of phase I trial of sorafenib in combination with dacarbazine in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2011, 68, 53–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mercatali, L.; Spadazzi, C.; Miserocchi, G.; Liverani, C.; De Vita, A.; Bongiovanni, A.; Recine, F.; Amadori, D.; Ibrahim, T. The effect of everolimus in an in vitro model of triple negative breast cancer and osteoclasts. Int. J. Mol. Sci. 2016, 17, 1827. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Vita, A.; Recine, F.; Mercatali, L.; Miserocchi, G.; Spadazzi, C.; Liverani, C.; Bongiovanni, A.; Pieri, F.; Casadei, R.; Riva, N.; et al. Primary Culture of Undifferentiated Pleomorphic Sarcoma: Molecular Characterization and Response to Anticancer Agents. Int. J. Mol. Sci. 2017, 18, 2662. https://doi.org/10.3390/ijms18122662
De Vita A, Recine F, Mercatali L, Miserocchi G, Spadazzi C, Liverani C, Bongiovanni A, Pieri F, Casadei R, Riva N, et al. Primary Culture of Undifferentiated Pleomorphic Sarcoma: Molecular Characterization and Response to Anticancer Agents. International Journal of Molecular Sciences. 2017; 18(12):2662. https://doi.org/10.3390/ijms18122662
Chicago/Turabian StyleDe Vita, Alessandro, Federica Recine, Laura Mercatali, Giacomo Miserocchi, Chiara Spadazzi, Chiara Liverani, Alberto Bongiovanni, Federica Pieri, Roberto Casadei, Nada Riva, and et al. 2017. "Primary Culture of Undifferentiated Pleomorphic Sarcoma: Molecular Characterization and Response to Anticancer Agents" International Journal of Molecular Sciences 18, no. 12: 2662. https://doi.org/10.3390/ijms18122662