Progressive Vascular Functional and Structural Damage in a Bronchopulmonary Dysplasia Model in Preterm Rabbits Exposed to Hyperoxia
Abstract
:1. Introduction
2. Results
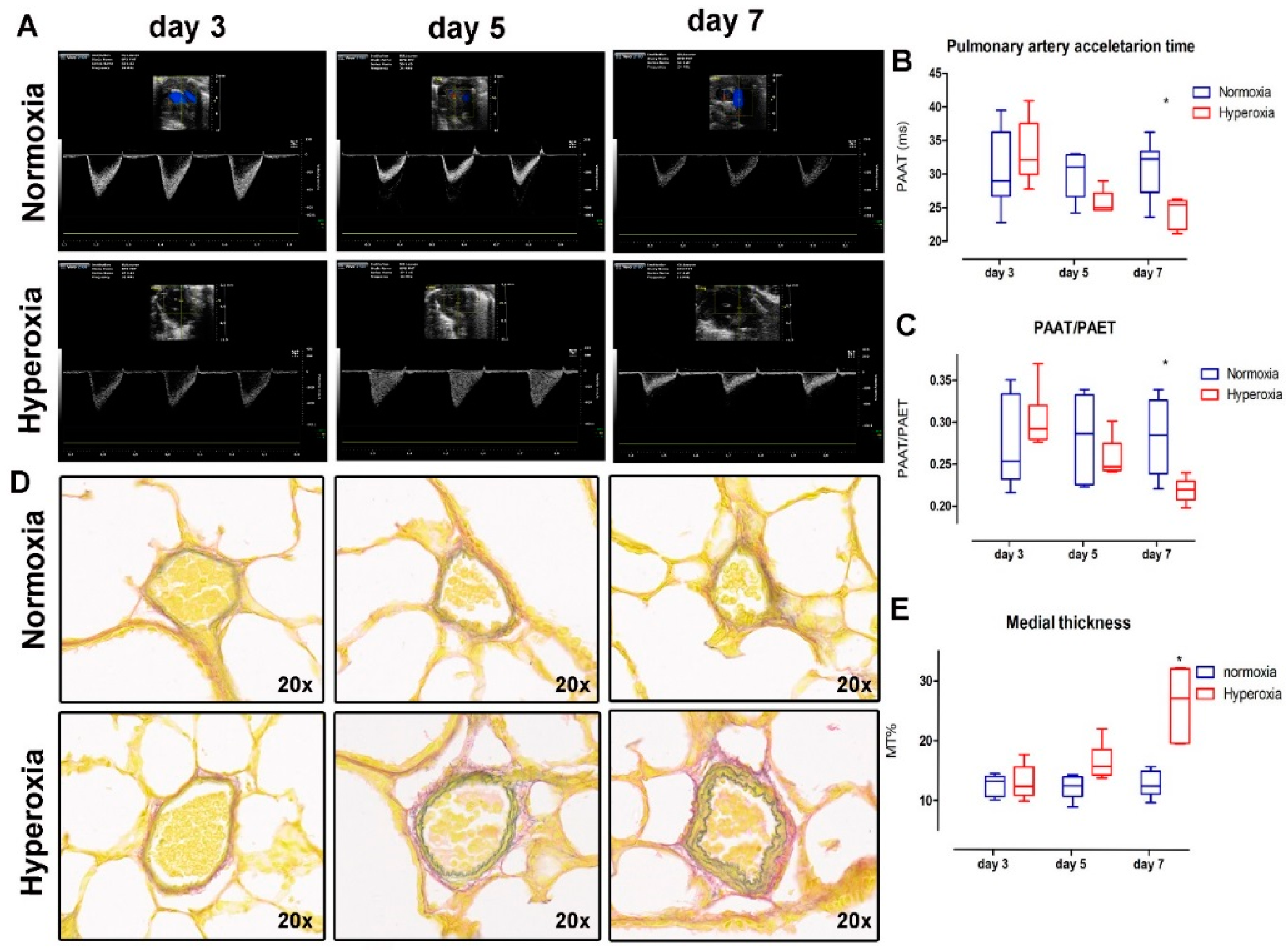
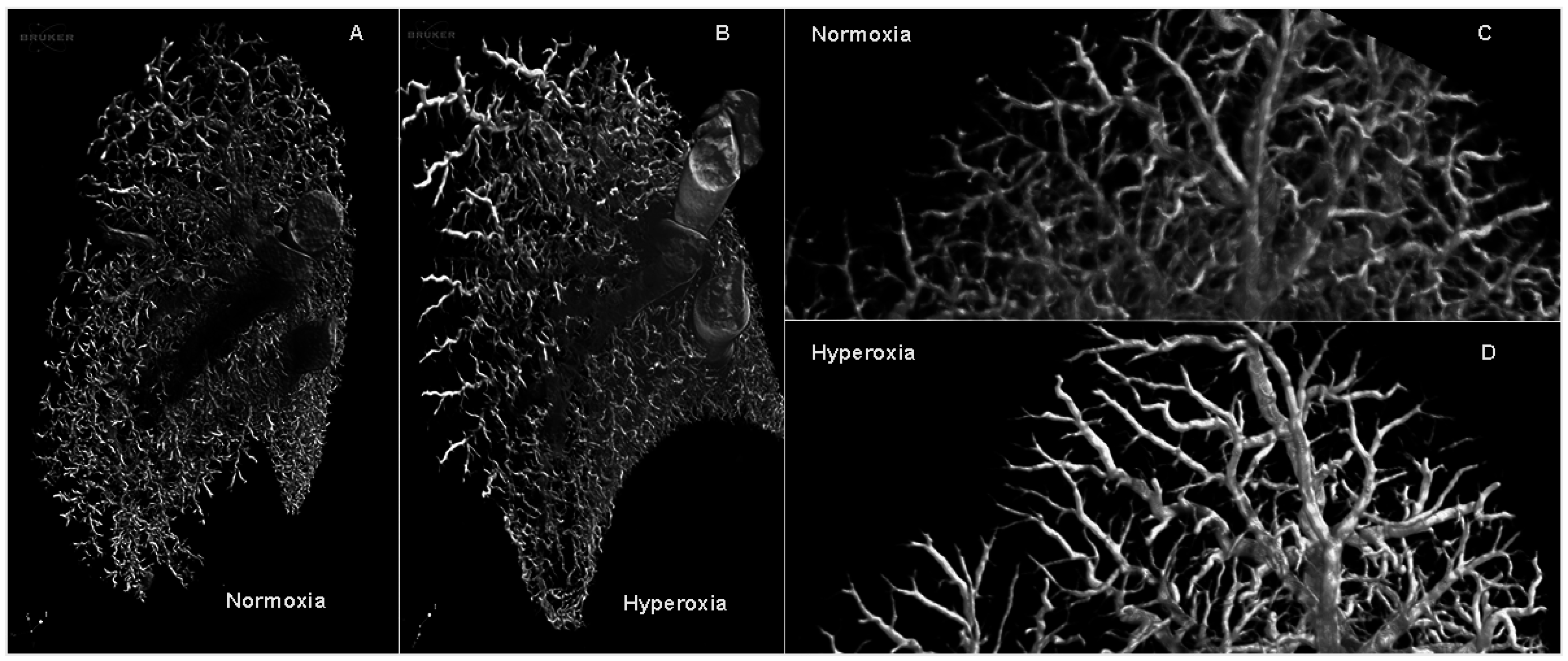
2.1. Vascular Changes: Hyperoxia Induces Lung Vasculature Changes and Results in Pulmonary Hypertension
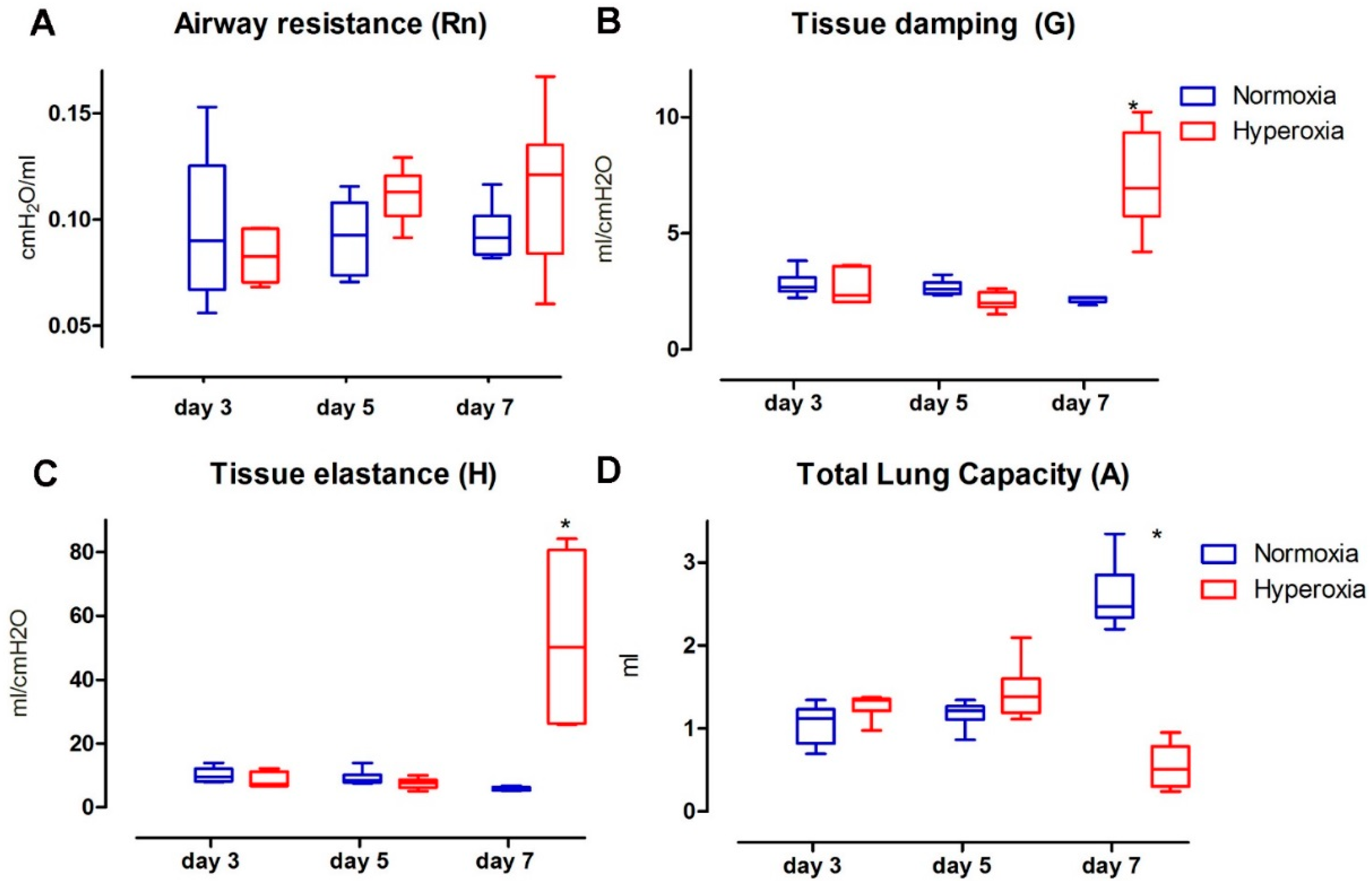
2.2. Functional Parenchymal Changes: Hyperoxia Causes Progressive Functional Changes in the Lung Parenchyma of Preterm Rabbits
2.3. Structural Changes in the Lung Parenchyma: Vascular Changes Are Related to Progressive Structural Changes in the Lung Parenchyma of Preterm Rabbits
3. Discussion
4. Materials and Methods
4.1. Animal Protocols
4.2. Pulmonary Artery Micro Ultrasound Doppler
4.3. Invasive Measurements
4.4. Lung Function Test
4.5. Histological Assessment of the Lungs
4.6. Barium Angiograms
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| A | Total lung capacity |
| BPD | Bronchopulmonary Dysplasia |
| BW | Body weight |
| Cst | Static compliance |
| ED | External diameter |
| G | Tissue damping |
| GA | Gestational age |
| H | Tissue elastance |
| H&E | Hematoxylin and eosin |
| ID | Internal diameter |
| LIS | Lung injury score system |
| Lm | Mean linear intercept |
| Lmw | Mean wall transection length |
| P8 | Primewave-8 perturbation |
| PAAT | Pulmonary artery acceleration time |
| PAET | Pulmonary artery ejection time |
| PAAT/PAET ratio | Pulmonary artery acceleration/ejection time ration |
| PN | Postnatal |
| PVr-V | Pressure volume perturbation |
| RAC | Radial alveolar count |
| Rn | Airway resistance |
| RVSP | Right ventricular systolic pressure |
References
- McEvoy, C.T.; Jain, L.; Schmidt, B.; Abman, S.; Bancalari, E.; Aschner, J.L. Bronchopulmonary dysplasia: Nhlbi workshop on the primary prevention of chronic lung diseases. Ann. Am. Thorac. Soc. 2014, 11, S146–S153. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Shankaran, S.; Laptook, A.R.; Walsh, M.C.; Hale, E.C.; Newman, N.S.; Schibler, K.; Carlo, W.A.; et al. Neonatal outcomes of extremely preterm infants from the nichd neonatal research network. Pediatrics 2010, 126, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Husain, A.N.; Siddiqui, N.H.; Stocker, J.T. Pathology of arrested acinar development in postsurfactant bronchopulmonary dysplasia. Hum. Pathol. 1998, 29, 710–717. [Google Scholar] [CrossRef]
- Jobe, A.H. Antenatal factors and the development of bronchopulmonary dysplasia. Semin. Neonatol. 2003, 8, 9–17. [Google Scholar] [CrossRef]
- Doyle, L.W. Evaluation of neonatal intensive care for extremely-low-birth-weight infants. Semin. Fetal Neonat. Med. 2006, 11, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Abman, S.H. The dysmorphic pulmonary circulation in bronchopulmonary dysplasia: A growing story. Am. J. Respir. Crit. Care Med. 2008, 178, 114–115. [Google Scholar] [CrossRef] [PubMed]
- Mourani, P.M.; Sontag, M.K.; Younoszai, A.; Ivy, D.D.; Abman, S.H. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics 2008, 121, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Mourani, P.M.; Abman, S.H. Pulmonary hypertension and vascular abnormalities in bronchopulmonary dysplasia. Clin. Perinatol. 2015, 42, 839–855. [Google Scholar] [CrossRef] [PubMed]
- Khemani, E.; McElhinney, D.B.; Rhein, L.; Andrade, O.; Lacro, R.V.; Thomas, K.C.; Mullen, M.P. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: Clinical features and outcomes in the surfactant era. Pediatrics 2007, 120, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- Berger, J.; Bhandari, V. Animal models of bronchopulmonary dysplasia. The term mouse models. Lung Cell. Mol. Physiol. 2014, 307, L936–L947. [Google Scholar] [CrossRef] [PubMed]
- D’Angio, C.T.; Ryan, R.M. Animal models of bronchopulmonary dysplasia. The preterm and term rabbit models. Lung Cell. Mol. Physiol. 2014, 307, L959–L969. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.; Thebaud, B. Animal models of bronchopulmonary dysplasia. The term rat models. Lung Cell. Mol. Physiol. 2014, 307, L948–L958. [Google Scholar] [CrossRef] [PubMed]
- Yoder, B.A.; Coalson, J.J. Animal models of bronchopulmonary dysplasia. The preterm baboon models. Lung Cell. Mol. Physiol. 2014, 307, L970–L977. [Google Scholar] [CrossRef] [PubMed]
- Jobe, A.H. Animal models, learning lessons to prevent and treat neonatal chronic lung disease. Front. Med. 2015, 2, 49. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.; Toelen, J.; Vanoirbeek, J.; Kakigano, A.; Dekoninck, P.; Verbeken, E.; Deprest, J. Functional assessment of hyperoxia-induced lung injury after preterm birth in the rabbit. Lung Cell. Mol. Physiol. 2014, 306, L277–L283. [Google Scholar] [CrossRef] [PubMed]
- Thibault, H.B.; Kurtz, B.; Raher, M.J.; Shaik, R.S.; Waxman, A.; Derumeaux, G.; Halpern, E.F.; Bloch, K.D.; Scherrer-Crosbie, M. Noninvasive assessment of murine pulmonary arterial pressure: Validation and application to models of pulmonary hypertension. Circ. Cardiovasc. Imaging 2010, 3, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Kitabatake, A.; Inoue, M.; Asao, M.; Masuyama, T.; Tanouchi, J.; Morita, T.; Mishima, M.; Uematsu, M.; Shimazu, T.; Hori, M.; et al. Noninvasive evaluation of pulmonary hypertension by a pulsed doppler technique. Circulation 1983, 68, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Salaets, T.; Richter, J.; Brady, P.; Jimenez, J.; Nagatomo, T.; Deprest, J.; Toelen, J. Transcriptome analysis of the preterm rabbit lung after seven days of hyperoxic exposure. PLoS ONE 2015, 10, e0136569. [Google Scholar] [CrossRef] [PubMed]
- Mourani, P.M.; Sontag, M.K.; Younoszai, A.; Miller, J.I.; Kinsella, J.P.; Baker, C.D.; Poindexter, B.B.; Ingram, D.A.; Abman, S.H. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 2014, 191, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Coalson, J.J.; Kuehl, T.J.; Escobedo, M.B.; Hilliard, J.L.; Smith, F.; Meredith, K.; Null, D.M., Jr.; Walsh, W.; Johnson, D.; Robotham, J.L. A baboon model of bronchopulmonary dysplasia. II. Pathologic features. Exp. Mol. Pathol. 1982, 37, 335–350. [Google Scholar] [CrossRef]
- Thebaud, B.; Ladha, F.; Michelakis, E.D.; Sawicka, M.; Thurston, G.; Eaton, F.; Hashimoto, K.; Harry, G.; Haromy, A.; Korbutt, G.; et al. Vascular endothelial growth factor gene therapy increases survival, promotes lung angiogenesis, and prevents alveolar damage in hyperoxia-induced lung injury: Evidence that angiogenesis participates in alveolarization. Circulation 2005, 112, 2477–2486. [Google Scholar] [CrossRef] [PubMed]
- Van Haaften, T.; Byrne, R.; Bonnet, S.; Rochefort, G.Y.; Akabutu, J.; Bouchentouf, M.; Rey-Parra, G.J.; Galipeau, J.; Haromy, A.; Eaton, F.; et al. Airway delivery of mesenchymal stem cells prevents arrested alveolar growth in neonatal lung injury in rats. Am. J. Respir. Crit. Care Med. 2009, 180, 1131–1142. [Google Scholar] [CrossRef] [PubMed]
- Hilgendorff, A.; O’Reilly, M.A. Bronchopulmonary dysplasia early changes leading to long-term consequences. Front. Med. 2015, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- May, C.; Kennedy, C.; Milner, A.D.; Rafferty, G.F.; Peacock, J.L.; Greenough, A. Lung function abnormalities in infants developing bronchopulmonary dysplasia. Arch. Dis. Child. 2011, 96, 1014–1019. [Google Scholar] [CrossRef] [PubMed]
- Jobe, A.J. The new BPD: An arrest of lung development. Pediatr. Res. 1999, 46, 641–643. [Google Scholar] [CrossRef] [PubMed]
- Allison, B.J.; Crossley, K.J.; Flecknoe, S.J.; Davis, P.G.; Morley, C.J.; Harding, R.; Hooper, S.B. Ventilation of the very immature lung in utero induces injury and bpd-like changes in lung structure in fetal sheep. Pediatr. Res. 2008, 64, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Mascaretti, R.S.; Mataloun, M.M.G.B.; Dolhnikoff, M.; Rebello, C.M. Lung morphometry, collagen and elastin content: Changes after hyperoxic exposure in preterm rabbits. Clinics 2009, 64, 1099–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogawa, J.; Saito, H. Hyaline membrane in the lung of premature newborn mammals. Study on the etiological factors. Nagoya Med. J. 1961, 7, 44–49. [Google Scholar] [PubMed]
- Frank, L.; Bucher, J.R.; Roberts, R.J. Oxygen toxicity in neonatal and adult animals of various species. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1978, 45, 699–704. [Google Scholar] [PubMed]
- Frank, L.; Groseclose, E.E. Preparation for birth into an O2-rich environment: The antioxidant enzymes in the developing rabbit lung. Pediatr. Res. 1984, 18, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.; Sosenko, I.R. Prenatal development of lung antioxidant enzymes in four species. J. Pediatr. 1987, 110, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Walther, F.J.; David-Cu, R.; Lopez, S.L. Antioxidant-surfactant liposomes mitigate hyperoxic lung injury in premature rabbits. Am. J. Physiol. 1995, 269, L613–L617. [Google Scholar] [PubMed]
- Matute-Bello, G.; Downey, G.; Moore, B.B.; Groshong, S.D.; Matthay, M.A.; Slutsky, A.S.; Kuebler, W.M. An official american thoracic society workshop report: Features and measurements of experimental acute lung injury in animals. Am. J. Respir. Cell Mol. Biol. 2011, 44, 725–738. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.C.; Chi, E.Y.; Wilson, C.B.; Truog, W.E.; Teh, E.C.; Hodson, W.A. Sequence of inflammatory cell migration into lung during recovery from hyaline membrane disease in premature newborn monkeys. Am. Rev. Respir. Dis. 1987, 135, 937–940. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.C.; Palmer, S.; Wilson, C.B.; Standaert, T.A.; Truog, W.E.; Murphy, J.H.; Hodson, W.A. Postnatal changes in lung phospholipids and alveolar macrophages in term newborn monkeys. Respir. Physiol. 1988, 73, 289–300. [Google Scholar] [CrossRef]
- Ladha, F.; Bonnet, S.; Eaton, F.; Hashimoto, K.; Korbutt, G.; Thebaud, B. Sildenafil improves alveolar growth and pulmonary hypertension in hyperoxia-induced lung injury. Am. J. Respir. Crit. Care Med. 2005, 172, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Roubliova, X.I.; Deprest, J.A.; Biard, J.M.; Ophalvens, L.; Gallot, D.; Jani, J.C.; van de Ven, C.P.; Tibboel, D.; Verbeken, E.K. Morphologic changes and methodological issues in the rabbit experimental model for diaphragmatic hernia. Histol. Histopathol. 2010, 25, 1105–1116. [Google Scholar] [PubMed]
- Cooney, T.P.; Thurlbeck, W.M. The radial alveolar count method of emery and mithal: A reappraisal 2—Intrauterine and early postnatal lung growth. Thorax 1982, 37, 580–583. [Google Scholar] [CrossRef] [PubMed]
- Roubliova, X.I.; Van der Biest, A.M.; Vaast, P.; Lu, H.; Jani, J.C.; Lewi, P.J.; Verbeken, E.K.; Tibboel, D.; Deprest, J.A. Effect of maternal administration of betamethasone on peripheral arterial development in fetal rabbit lungs. Neonatology 2008, 93, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Langheinrich, A.C.; Leithauser, B.; Greschus, S.; Von Gerlach, S.; Breithecker, A.; Matthias, F.R.; Rau, W.S.; Bohle, R.M. Acute rat lung injury: Feasibility of assessment with micro-CT. Radiology 2004, 233, 165–171. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Measurment | Normoxia | Hyperoxia | ||||
|---|---|---|---|---|---|---|---|
| Day 3 | Day 5 | Day 7 | Day 3 | Day 5 | Day 7 | ||
| Pulmonary Artery Ultrasound and Histology | Pulmonary artery acceleration time (PAAT) ms ± SD 1 | 31.73 ± 6.682 | 31.28 ± 2.687 | 32.34 ± 3.240 2 | 33.5 ± 5.17 | 25.69 ± 1.859 | 25.03 ± 1.749 2 |
| Pulmonary artery acceleration/ejection time ratio (PAAT/PAET)% ± SD 3 | 28.47 ± 5.34 | 30.48 ± 3.128 | 29.92 ± 3.653 2 | 30.58 ± 3.742 | 26.03 ± 2.478 | 24.19 ± 3.229 2 | |
| Media thickness % (MT%) 4 | 12.57 ± 1.827 | 12.42 ± 2.077 | 12.83 ± 2.171 2 | 13.12 ± 5.059 | 14.56 ± 3.325 | 16.58 ± 2.979 2 | |
| Flexivent Parameter | Airway resistance (Rn) cmH2O/mL ± SD | 0.095 ± 0.014 | 0.091 ± 0.007 | 0.093 ± 0.005 | 0.082 ± 0.004 | 0.111 ± 0.005 | 0.124 ± 0.016 |
| Tissue damping (G) cmH2O/mL ± SD 4 | 2.736 ± 0.474 | 2.630 ± 0.351 | 2.162 ± 0.133 2 | 2.665 ± 0.742 | 2.079 ± 0.387 | 7.069 ± 1.967 2 | |
| Tissue elastance (H) cmH2O/mL ± SD 4 | 10.40 ± 3.116 | 9.314 ± 2.655 | 5.927 ± 0.533 2 | 8.551 ± 2.379 | 7.512 ± 1.671 | 49.25 ± 8.5 2 | |
| Total lung capacity (A) mL ± SD 5 | 1.1 ± 0.186 | 1.178 ± 0.163 | 2.593 ± 0.401 2 | 1.278 ± 0.149 | 1.455 ± 0.324 | 0.545 ± 0.256 2 | |
| Static compliance (Cst) mL/cmH2O ± SD 6 | 0.051 ± 0.013 | 0.061 ± 0.008 | 0.134 ± 0.021 2 | 0.067 ± 0.015 | 0.078 ± 0.033 | 0.025 ± 0.01 2 | |
| Histology Parenchymal | Linear intercept (Lm) ± SD 7 | 81.87 ± 7.342 | 73.48 ± 9.204 | 67.66 ± 2.883 | 87.39 ± 11.45 | 91.71 ± 8.006 | 96.58 ± 5.229 |
| Mean wall thickness (Lmw) ± SD 4 | 7.927 ± 1.56 | 7.673 ± 0.676 | 7.609 ± 0.691 2 | 8.859 ± 2.788 | 8.441 ± 1.818 | 22.76 ± 5.35 2 | |
| Radial alveolar count (RAC) ± SD 8 | 6.287 ± 0.365 | 6.528 ± 0.711 2 | 7.756 ± 0.471 2 | 5.717 ± 0.415 2 | 5.692 ± 0.562 2 | 4.715 ± 0.418 2 | |
| Acute lung inflammation score (ALI) ± SD 9 | 0.157 ± 0.093 | 0.281 ± 0.049 2 | 0.423 ± 0.069 2 | 0.305 ± 0.188 | 0.484 ± 0.159 2 | 0.659 ± 0.036 2 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez, J.; Richter, J.; Nagatomo, T.; Salaets, T.; Quarck, R.; Wagennar, A.; Wang, H.; Vanoirbeek, J.; Deprest, J.; Toelen, J. Progressive Vascular Functional and Structural Damage in a Bronchopulmonary Dysplasia Model in Preterm Rabbits Exposed to Hyperoxia. Int. J. Mol. Sci. 2016, 17, 1776. https://doi.org/10.3390/ijms17101776
Jiménez J, Richter J, Nagatomo T, Salaets T, Quarck R, Wagennar A, Wang H, Vanoirbeek J, Deprest J, Toelen J. Progressive Vascular Functional and Structural Damage in a Bronchopulmonary Dysplasia Model in Preterm Rabbits Exposed to Hyperoxia. International Journal of Molecular Sciences. 2016; 17(10):1776. https://doi.org/10.3390/ijms17101776
Chicago/Turabian StyleJiménez, Julio, Jute Richter, Taro Nagatomo, Thomas Salaets, Rozenn Quarck, Allard Wagennar, Hongmei Wang, Jeroen Vanoirbeek, Jan Deprest, and Jaan Toelen. 2016. "Progressive Vascular Functional and Structural Damage in a Bronchopulmonary Dysplasia Model in Preterm Rabbits Exposed to Hyperoxia" International Journal of Molecular Sciences 17, no. 10: 1776. https://doi.org/10.3390/ijms17101776






