Clonal Expansion of T Cells in Abdominal Aortic Aneurysm: A Role for Doxycycline as Drug of Choice?
Abstract
:1. Introduction
2. Pharmacological Interventions for AAA
3. Doxycycline and AAA
| Targets | Pharmacological Approaches | References |
|---|---|---|
| Neutrophils and other blood components | Anti-neutrophil antibodies, TNF-α inhibition, mycophenolate | [21–28] this review |
| β-Adrenergic blockade | Propranolol | [29–33] |
| Renin-angiotensin system | TGF-β1, cyclosporine A | [22,24,28,34–47] |
| Cholesterol metabolism | Various statins and proteases | [43,47–57] |
| Phospholipid metabolism | 5-LO inhibitors, cyclooxygenase-2 inhibitors, EP4 inhibitors | [26,28,58–64] |
| Peroxisome proliferation-associated receptor (PPAR) | Glitazones | [65,66] |
| Various proteases: cysteine proteases, serine proteases, matrix metalloproteinases (MMPs), elastase and others | Calpain inhibitors, chymase inhibitors, doxycycline, azithromycin, rhoxithromycin | [24,25,33,39,41,67–70] this review |
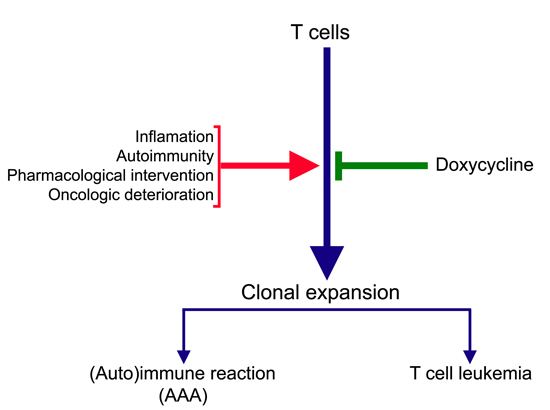
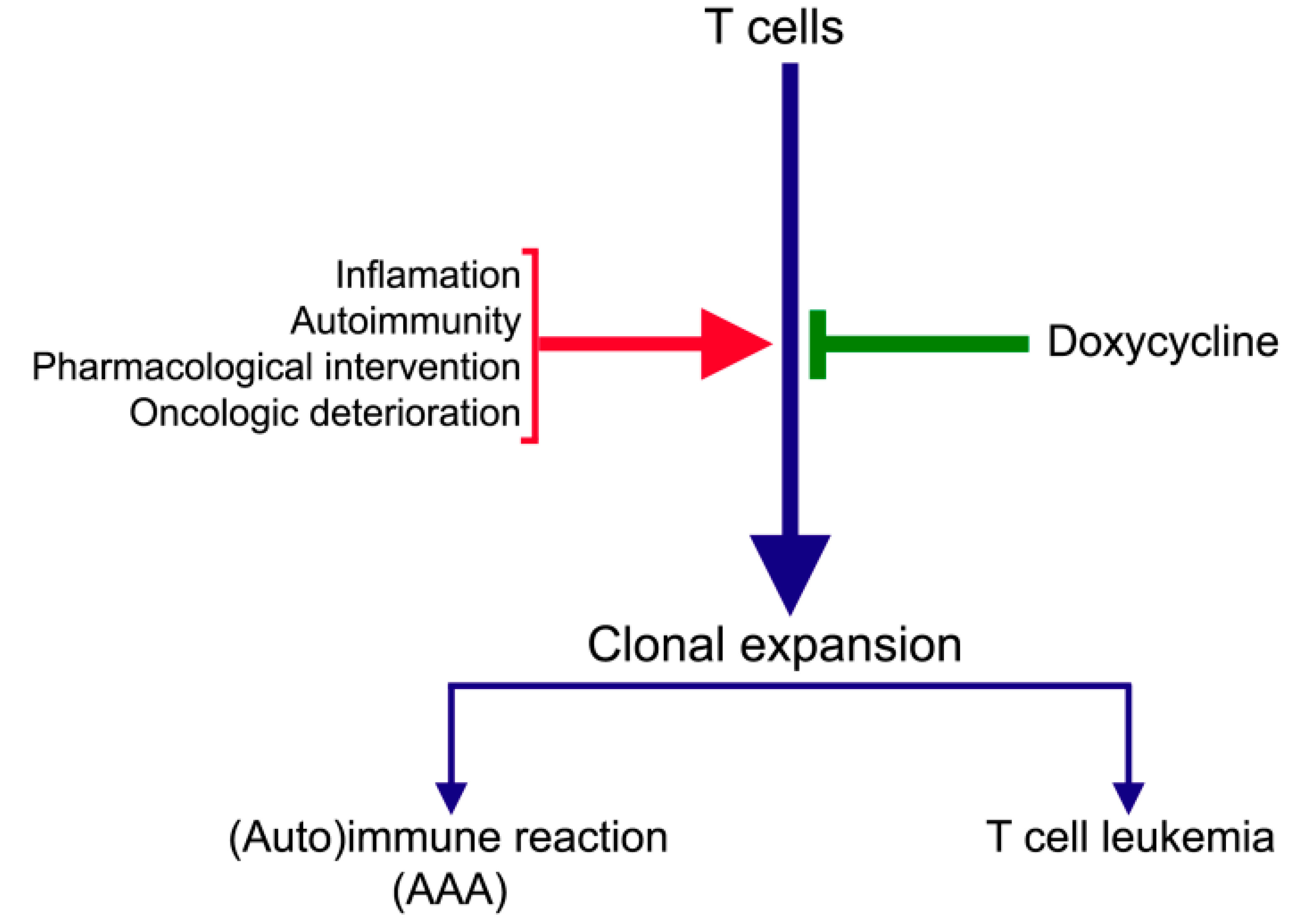
4. Doxycycline and Inhibition of T Cell Clonal Expansion
5. Doxycycline and Inhibition of Matrix Metalloproteinases (MMPs)
6. Doxycycline in Cell Culture and Animal Models of AAA
| Publication | Doxycycline | No. of Animals | Study Parameters | Effect | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1st Author (Year) | Ref. | Dosage | Serum Level | Type | Duration | Methods | Outcomes | ||
| Petrinec, D. (1996) | [90] | 12.5 mg bid, s.c. | No data | 48 rats | PC | ≤14 days | el.-ind. AAA | MMP exp.; MMP act.; expansion | + |
| Boyle, J.R. (1998) | [91] | 1 and 10 µg/mL | NA | 8 porcine samples | In vitro | 13 days | el.-ind. AAA | MMP exp.; MMP act | + |
| Curci, J.A. (1998) | [92] | n.s., s.c. | No data | 52 rats | Open controlled | 7 days | el.-ind. AAA | MMP exp.; MMP act.; expansion | + |
| Prall, A.K. (2002) | [87] | 10, 50, 100 mg/kg/d in d.w. | 1.4, 2.7, 11.9 µg/mL | n.s. (mice) | Open PC | 10 weeks | el.-ind. AAA | MMP exp.; expansion | + |
| Manning, M.W. (2003) | [93] | 30 mg/kg/d in d.w. | No data | 60 mice (hyperlipidemic) | PC | 5 weeks | ang. II-ind. AAA | Expansion | + |
| Sho, E. (2004) | [94] | 60 mg/kg/d, s.c.; 1.5 mg/kg/d via infusion | No data | n.s. (rats) | PC Controlled | 14 days | el.-ind. AAA; periaortic infusion | MMP exp.; expansion; macrophage density | + |
| Bartoli, M.A. (2006) | [95] | 100 mg/kg/d systemic p.o. | 0.33 µg/mL | n.s. (mice) | Open comparative | 14 days | el.-ind. AAA | Expansion | + |
| ≤1 mg/kg/d via local infusion | 5.6‒7.8 ng/mL | n.s. (mice) | Open comparative | 14 days | el.-ind. AAA; localised infusion with osmotic minipump | Expansion | + | ||
| Xiong, W. (2008) | [89] | 100 mg/kg/d in d.w. | No data | 48 mice | Open PC | 6 weeks + follow-up | Marfan syndrome | Survival | + |
| Xie, X. (2012) | [96] | 100 mg/kg/d in d.w. | 2.3 ± 0.6 μg/mL | 25 mice | PC | 8 weeks | ang. II-ind. AAA | Expansion | – |
| Sivaraman, B. (2013) | [97] | 2%, 5% and 10% in nanoparticles | NA | n.s. (rat AAA tissue) | In vitro | Rats: 2 weeks TC: 3 weeks | el.-ind. AAA | MMP exp.; MMP act | + |
7. Doxycycline in Clinical Trials of AAA Patients
| Publication | Doxycycline | Study Parameters | ||||||
|---|---|---|---|---|---|---|---|---|
| 1st Author (Year) | Ref. | Dosage | Serum Level | No. of Patients | Type | Duration | Outcomes | Effect |
| Thompson, R.W. (1999) | [99] | 100 mg 2× dd | No data | 10 | Open | 7 days | Small AAA | + |
| Curci, J.A. (2000) | [86] | 100 mg 2× dd | No data | 15 | Open controlled | 7 days | MMP exp. | + |
| Mosorin, M. (2001) | [100] | 150 mg 1× dd | No data | 32 | DBPC | 3 months +15 months | Expansion, 15 months surveillance | + |
| Baxter, B.T. (2002) | [101] | 100 mg 2× dd | 4.62 µg/mL | 36 | DBPC Phase II | 6 months | MMP exp.; expansion | +; − |
| Prall, A.K. (2002) | [87] | 100 mg 2× dd | 1.8–9.2 µg/mL | n.s. | Open | 6 months | Serum levels in range of those of mice in comparative study (see Table 2) | + |
| Brown, D.L. (2004) | [102] | 20 mg 2× dd | No data | 50 | DBPC | 6 months | Acute coronary syndromes, MMP exp. | No AAA |
| Hackmann, A.E. (2008) | [68] | 100 mg 2× dd | No data | 44 | DBPC | 6 months | MMP exp.; expansion | +; + |
| Lindeman, J.H.N. (2009) | [20] | 50, 100, 300 mg 1× dd | No data | 60 | SB controlled | 2 weeks | MMP exp.; MMP act; leukocyte content | +; ±; + |
| Meijer, C.A. (2013) | [103] | 100 mg 1× dd | No data | 286 | DBPC | 18 months | Expansion | − |
| Kurosawa, K. (2013) | [10,104] | 100 mg 2× dd | No data | 248 | DBPC | 2–3 years (planned) | Study in progress | unkown |
8. Direct and Indirect Effects of Doxycycline
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lindholt, J.S. Abdominal aortic aneurysms. Dan. Med. Bull. 2010, 57, B4219. [Google Scholar] [PubMed]
- NHS Abdominal Aortic Screening Programme. Available online: http://www.aaa.screening.nhs.uk/2013–14datareports (accessed on 28 November 2014).
- Khosla, S.; Morris, D.R.; Moxon, J.V.; Walker, P.J.; Gasser, T.C.; Golledge, J. Meta-analysis of peak wall stress in ruptured, symptomatic and intact abdominal aortic aneurysms. Br. J. Surg. 2014, 101, 1350–1357. [Google Scholar] [CrossRef] [PubMed]
- Sweeting, M.J.; Thompson, S.G.; Brown, L.C.; Powell, J.T. Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br. J. Surg. 2012, 99, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.T.; Brown, L.C.; Greenhalgh, R.M.; Thompson, S.G. The rupture rate of large abdominal aortic aneurysms: Is this modified by anatomical suitability for endovascular repair? Ann. Surg. 2008, 247, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Lederle, F.A.; Freischlag, J.A.; Kyriakides, T.C.; Padberg, F.T., Jr.; Matsumura, J.S.; Kohler, T.R.; Lin, P.H.; Jean-Claude, J.M.; Cikrit, D.F.; Swanson, K.M.; et al. Outcomes following endovascular vs. open repair of abdominal aortic aneurysm: A randomized trial. JAMA 2009, 302, 1535–1542. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, G.A.; Georgiadis, G.S.; Antoniou, S.A.; Pavlidis, P.; Maras, D.; Sfyroeras, G.S.; Georgakarakos, E.I.; Lazarides, M.K. Endovascular repair for ruptured abdominal aortic aneurysm confers an early survival benefit over open repair. J. Vasc. Surg. 2013, 58, 1091–1105. [Google Scholar] [CrossRef] [PubMed]
- Baxter, B.T.; Terrin, M.C.; Dalman, R.L. Medical management of small abdominal aortic aneurysms. Circulation 2008, 117, 1883–1889. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Rateri, D.L.; Bruemmer, D.; Cassis, L.A.; Daugherty, A. Novel mechanisms of abdominal aortic aneurysms. Curr. Atheroscler. Rep. 2012, 14, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, K.; Matsumura, J.S.; Yamanouchi, D. Current status of medical treatment for abdominal aortic aneurysm. Circ. J. 2013, 77, 2860–2866. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; White, J.V.; Lin, W.L.; Zhang, X.; Solomides, C.; Evans, K.; Ntaoula, N.; Nwaneshiudu, I.; Gaughan, J.; Monos, D.S.; et al. Aneurysmal lesions of patients with abdominal aortic aneurysm contain clonally expanded T cells. J. Immunol. 2014, 192, 4897–4912. [Google Scholar] [CrossRef] [PubMed]
- Kroon, A.M.; Taanman, J.W. Comment on “Aneurysmal lesions of patients with abdominal aortic aneurysm contain clonally expanded T cells”. J. Immunol. 2014, 193, 2041. [Google Scholar] [CrossRef] [PubMed]
- Kroon, A.M.; Taanman, J.W. Mitochondria and cancer: The Warburg fact. Chemotherapy 2014, 3, 314. [Google Scholar]
- Shimizu, K.; Shichiri, M.; Libby, P.; Lee, R.T.; Mitchell, R.N. Th2-predominant inflammation and blockade of IFN-γ signaling induce aneurysms in allografted aortas. J. Clin. Investig. 2004, 114, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Uchida, H.A.; Kristo, F.; Rateri, D.L.; Lu, H.; Charnigo, R.; Cassis, L.A.; Daugherty, A. Total lymphocyte deficiency attenuates AngII-induced atherosclerosis in males but not abdominal aortic aneurysms in apoE deficient mice. Atherosclerosis 2010, 211, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.; Zhang, J.; Wang, Y.; Wang, S.; Bockler, D.; Duan, Z.; Xin, S. Deficient CD4+CD25+ T regulatory cell function in patients with abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 1825–1831. [Google Scholar] [CrossRef] [PubMed]
- Platsoucas, C.D.; Lu, S.; Nwaneshiudu, I.; Solomides, C.; Agelan, A.; Ntaoula, N.; Purev, E.; Li, L.P.; Kratsios, P.; Mylonas, E.; et al. Abdominal aortic aneurysm is a specific antigen-driven T cell disease. Ann. N. Y. Acad. Sci. 2006, 1085, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, M.; Duftner, C.; Seiler, R.; Dejaco, C.; Fraedrich, G. Abdominal aortic aneurysms: An underestimated type of immune-mediated large vessel arteritis? Curr. Opin. Rheumatol. 2006, 18, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Platsoucas, C.D.; Oleszak, E.L. Human autoimmune diseases are specific antigen-driven T-cell diseases: Identification of the antigens. Immunol. Res. 2007, 38, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, J.H.N; Abdul-Hussien, H.; van Bockel, J.H.; Wolterbeek, R.; Kleemann, R. Clinical trial of doxycycline for matrix metalloproteinase-9 inhibition in patients with an abdominal aneurysm: Doxycycline selectively depletes aortic wall neutrophils and cytotoxic T cells. Circulation 2009, 119, 2209–2216. [Google Scholar] [CrossRef] [PubMed]
- Xiong, W.; MacTaggart, J.; Knispel, R.; Worth, J.; Persidsky, Y.; Baxter, B.T. Blocking TNF-α attenuates aneurysm formation in a murine model. J. Immunol. 2009, 183, 2741–2746. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, J.H.N.; Rabelink, T.J.; van Bockel, J.H. Immunosuppression and the abdominal aortic aneurysm: Doctor Jekyll or Mister Hyde? Circulation 2011, 124, e463–e465. [Google Scholar] [CrossRef] [PubMed]
- Kimura, H.; Akutsu, N.; Shiomi, R.; Kohmura, E. Subarachnoid hemorrhage caused by ruptured intracranial fusiform aneurysm associated with microscopic polyangiitis. Neurol. Med. Chir. (Tokyo) 2012, 52, 495–498. [Google Scholar] [CrossRef]
- Shi, G.P.; Lindholt, J.S. Mast cells in abdominal aortic aneurysms. Curr. Vasc. Pharmacol. 2013, 11, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Shi, G.P. Mast cell chymase and tryptase in abdominal aortic aneurysm formation. Trends Cardiovasc. Med. 2012, 22, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Hansson, E.C.; Dellborg, M.; Lepore, V.; Jeppsson, A. Prevalence, indications and appropriateness of antiplatelet therapy in patients operated for acute aortic dissection: Associations with bleeding complications and mortality. Heart 2013, 99, 116–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alsac, J.M.; Delbosc, S.; Rouer, M.; Journé, C.; Louedec, L.; Meilhac, O.; Michel, J.B. Fucoidan interferes with Porphyromonas gingivalis-induced aneurysm enlargement by decreasing neutrophil activation. J. Vasc. Surg. 2013, 57, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Yang, J.; Zhang, K.; An, G.; Kong, J.; Jiang, F.; Zhang, Y.; Zhang, C. Regulatory T cells prevent angiotensin II-induced abdominal aortic aneurysm in apolipoprotein E knockout mice. Hypertension 2014, 64, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Leach, S.D.; Toole, A.L.; Stern, H.; DeNatale, R.W.; Tilson, M.D. Effect of β-adrenergic blockade on the growth rate of abdominal aortic aneurysms. Arch. Surg. 1988, 123, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Gadowski, G.R.; Pilcher, D.B.; Ricci, M.A. Abdominal aortic aneurysm expansion rate: Effect of size and β-adrenergic blockade. J. Vasc. Surg. 1994, 19, 727–731. [Google Scholar] [CrossRef] [PubMed]
- Lindholt, J.S.; Henneberg, E.W.; Juul, S.; Fasting, H. Impaired results of a randomised double blinded clinical trial of propranolol versus placebo on the expansion rate of small abdominal aortic aneurysms. Int. Angiol. 1999, 18, 52–57. [Google Scholar] [PubMed]
- Guessous, I.; Periard, D.; Lorenzetti, D.; Cornuz, J.; Ghali, W.A. The efficacy of pharmacotherapy for decreasing the expansion rate of abdominal aortic aneurysms: A systematic review and meta-analysis. PLoS ONE 2008, 3, e1895. [Google Scholar] [CrossRef] [PubMed]
- Rughani, G.; Robertson, L.; Clarke, M. Medical treatment for small abdominal aortic aneurysms. Cochrane Database Syst. Rev. 2012. [CrossRef]
- Liao, S.; Miralles, M.; Kelley, B.J.; Curci, J.A.; Borhani, M.; Thompson, R.W. Suppression of experimental abdominal aortic aneurysms in the rat by treatment with angiotensin-converting enzyme inhibitors. J. Vasc. Surg. 2001, 33, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Neptune, E.R.; Frischmeyer, P.A.; Arking, D.E.; Myers, L.; Bunton, T.E.; Gayraud, B.; Ramirez, F.; Sakai, L.Y.; Dietz, H.C. Dysregulation of TGF-β activation contributes to pathogenesis in Marfan syndrome. Nat. Genet. 2003, 33, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Habashi, J.P.; Judge, D.P.; Holm, T.M.; Cohn, R.D.; Loeys, B.L.; Cooper, T.K.; Myers, L.; Klein, E.C.; Liu, G.; Calvi, C.; et al. Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science 2006, 312, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, A.; Manning, M.W.; Cassis, L.A. Angiotensin II promotes atherosclerotic lesions and aneurysms in apolipoprotein E-deficient mice. J. Clin. Investig. 2000, 105, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Sweeting, M.J.; Thompson, S.G.; Brown, L.C.; Greenhalgh, R.M.; Powell, J.T. Use of angiotensin converting enzyme inhibitors is associated with increased growth rate of abdominal aortic aneurysms. J. Vasc. Surg. 2010, 52, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, V.; Uchida, H.A.; Ijaz, T.; Moorleghen, J.J.; Howatt, D.A.; Balakrishnan, A. Calpain inhibition attenuates angiotensin II-induced abdominal aortic aneurysms and atherosclerosis in low-density lipoprotein receptor-deficient mice. J. Cardiovasc. Pharmacol. 2012, 59, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Rateri, D.L.; Bruemmer, D.; Cassis, L.A.; Daugherty, A. Involvement of the renin-angiotensin system in abdominal and thoracic aortic aneurysms. Clin. Sci. (Lond.) 2012, 123, 531–543. [Google Scholar] [CrossRef]
- Takai, S.; Jin, D.; Miyazaki, M. Multiple mechanisms for the action of chymase inhibitors. J. Pharmacol. Sci. 2012, 118, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Groenink, M.; den Hartog, A.W.; Franken, R.; Radonic, T.; de Waard, V.; Timmermans, J.; Scholte, A.J.; van den Berg, M.P.; Spijkerboer, A.M.; Marquering, H.A.; et al. Losartan reduces aortic dilatation rate in adults with Marfan syndrome: A randomized controlled trial. Eur. Heart J. 2013, 34, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- Piechota-Polanczyk, A.; Demyanets, S.; Nykonenko, O.; Huk, I.; Mittlboeck, M.; Domenig, C.M.; Neumayer, C.; Wojta, J.; Nanobachvili, J.; Klinger, M. Decreased tissue levels of cyclophilin A, a cyclosporine A target and phospho-ERK1/2 in simvastatin patients with abdominal aortic aneurysm. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.F.; Yan, H.; Bertram, P.; Hu, Y.; Springer, L.E.; Thompson, R.W.; Curci, J.A.; Hourcade, D.E.; Pham, C.T. Fibrinogen-specific antibody induces abdominal aortic aneurysm in mice through complement lectin pathway activation. Proc. Natl. Acad. Sci. USA 2013, 110, E4335–E4344. [Google Scholar] [CrossRef] [PubMed]
- Sharif, M.A.; McDowell, D.A.; Badger, S.A. Chlamydia pneumoniae antibodies and C-reactive protein levels in patients with abdominal aortic aneurysms. Sci. World J. 2013, doi:org/10.1155/2013/212450.
- Wheeler, J.B.; Ikonomidis, J.S.; Jones, J.A. Connective tissue disorders and cardiovascular complications: The indomitable role of transforming growth factor-β signaling. Adv. Exp. Med. Biol. 2014, 802, 107–127. [Google Scholar] [PubMed]
- Takahashi, K.; Matsumoto, Y.; Doe, Z.; Kanazawa, M.; Satoh, K.; Shimizu, T.; Sato, A.; Fukumoto, Y.; Shimokawa, H. Combination therapy with atorvastatin and amlodipine suppresses angiotensin II-induced aortic aneurysm formation. PLoS ONE 2013, 8, e72558. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, E.F.; Buckley, C.; Shames, M.L.; Ennis, T.L.; Vanvickle-Chavez, S.J.; Mao, D.; Goeddel, L.A.; Hawkins, C.J.; Thompson, R.W. Treatment with simvastatin suppresses the development of experimental abdominal aortic aneurysms in normal and hypercholesterolemic mice. Ann. Surg. 2005, 241, 92–101. [Google Scholar] [PubMed]
- Schouten, O.; van Laanen, J.H.H.; Boersma, E.; Vidakovic, R.; Feringa, H.H.H.; Dunkelgrűn, M.; Bax, J.J.; Koning, J.; van Urk, H.; Poldermans, D. Statins are associated with a reduced infrarenal abdominal aortic aneurysm growth. Eur. J. Vasc. Endovasc. Surg. 2006, 32, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Powell, J.T.; Schwalbe, E.; Loftus, I.M.; Thompson, M.M. Simvastatin attenuates the activity of matrix metalloprotease-9 in aneurysmal aortic tissue. Eur. J. Vasc. Endovasc. Surg. 2007, 34, 302–303. [Google Scholar] [CrossRef] [PubMed]
- Takagi, H.; Matsui, M.; Umemoto, T. A meta-analysis of clinical studies of statins for prevention of abdominal aortic aneurysm expansion. J. Vasc. Surg. 2010, 52, 1675–1681. [Google Scholar] [CrossRef] [PubMed]
- Takagi, H.; Yamamoto, H.; Iwata, K.; Goto, S.; Umemoto, T. Effects of statin therapy on abdominal aortic aneurysm growth: A meta-analysis and meta-regression of observational comparative studies. Eur. J. Vasc. Endovasc. Surg. 2012, 44, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Mastoraki, S.T.; Toumpoulis, I.K.; Anagnostopoulos, C.E.; Tiniakos, D.; Papalois, A.; Chamogeorgakis, T.P.; Angouras, D.C.; Rokkas, C.K. Treatment with simvastatin inhibits the formation of abdominal aortic aneurysms in rabbits. Ann. Vasc. Surg. 2012, 26, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Piechota-Polanczyk, A.; Goraca, A.; Demyanets, S.; Mittlboeck, M.; Domenig, C.; Neumayer, C.; Wojta, J.; Nanobachvili, J.; Huk, I.; Klinger, M. Simvastatin decreases free radicals formation in the human abdominal aortic aneurysm wall via NF-κB. Eur. J. Vasc. Endovasc. Surg. 2012, 44, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Van der Meij, E.; Koning, G.G.; Vriens, P.W.; Peeters, M.F.; Meijer, C.A.; Kortekaas, K.E.; Dalman, R.L.; van Bockel, J.H.; Hanemaaijer, R.; Kooistra, T.; et al. A clinical evaluation of statin pleiotropy: Statins selectively and dose-dependently reduce vascular inflammation. PLoS ONE 2013, 8, e53882. [Google Scholar] [CrossRef] [PubMed]
- Houdek, K.; Moláček, J.; Třeška, V.; Križkova, V.; Eberlová, L.; Boudová, L.; Nedorost, L.; Tolinger, P.; Kočová, J.; Kobr, J.; et al. Focal histopathological progression of porcine experimental abdominal aortic aneurysm is mitigated by atorvastatin. Int. Angiol. 2013, 32, 291–306. [Google Scholar] [PubMed]
- Twine, C.P.; Williams, I.M. Comment on: “Effects of statin therapy on abdominal aortic aneurysm growth: A meta-analysis and meta-regression of observational comparative studies”. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 98. [Google Scholar] [CrossRef] [PubMed]
- Kristo, F.; Hardy, G.J.; Anderson, T.J.; Sinha, S.; Ahluwalia, N.; Lin, A.Y.; Passeri, J.; Scherrer-Crosbie, M.; Gerszten, R.E. Pharmacological inhibition of BLT1 diminishes early abdominal aneurysm formation. Atherosclerosis 2010, 210, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Ghoshal, S.; Loftin, C.D. Cyclooxygenase-2 inhibition attenuates abdominal aortic aneurysm progression in hyperlipidemic mice. PLoS ONE 2012, 7, e44369. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, K.; Gitlin, J.M.; Loftin, C.D. Effectiveness of cyclooxygenase-2 inhibition in limiting abdominal aortic aneurysm progression in mice correlates with a differentiated smooth muscle cell phenotype. J. Cardiovasc. Pharmacol. 2012, 60, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Samson, R. Can pharmacologic agents slow abdominal aortic aneurysm growth? Semin. Vasc. Surg. 2012, 25, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Scully, M.; Gang, C.; Condron, C.; Bouchier-Hayes, D.; Cunningham, A.J. Protective role of cyclooxygenase (COX)-2 in experimental lung injury: Evidence of a lipoxin A4-mediated effect. J. Surg. Res. 2012, 175, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, U.; Ishiwata, R.; Jin, M.H.; Kato, Y.; Suzuki, O.; Jin, H.; Ichikawa, Y.; Kumagaya, S.; Katayama, Y.; Fujita, T.; et al. Inhibition of EP4 signaling attenuates aortic aneurysm formation. PLoS ONE 2012, 7, e36724. [Google Scholar] [CrossRef] [PubMed]
- Duftner, C.; Seiler, R.; Dejaco, C.; Chemelli-Steingruber, I.; Schennach, H.; Klotz, W.; Rieger, M.; Herold, M.; Falkensammer, J.; Fraedrich, G.; et al. Antiphospholipid antibodies predict progression of abdominal aortic aneurysms. PLoS ONE 2014, 9, e99302. [Google Scholar] [CrossRef] [PubMed]
- Kadowaki, T. PPARγ agonist and antagonist. Nihon Yakurigaku. Zasshi. 2001, 118, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Torsney, E.; Pirianov, G.; Cockerill, G.W. Diabetes as a negative risk factor for abdominal aortic aneurysm—Does the disease aetiology or the treatment provide the mechanism of protection? Curr. Vasc. Pharmacol. 2013, 11, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Vammen, S.; Lindholt, J.S.; Ostergaard, L.; Fasting, H.; Henneberg, E.W. Randomized double-blind controlled trial of roxithromycin for prevention of abdominal aortic aneurysm expansion. Br. J. Surg. 2001, 88, 1066–1072. [Google Scholar] [CrossRef] [PubMed]
- Hackmann, A.E.; Rubin, B.G.; Sanchez, L.A.; Geraghty, P.A.; Thompson, R.W.; Curci, J.A. A randomized, placebo-controlled trial of doxycycline after endoluminal aneurysm repair. J. Vasc. Surg. 2008, 48, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, L.; Gnarpe, J.; Bergqvist, D.; Lindbäck, J.; Pärsson, H. The effect of azithromycin and Chlamydophilia pneumonia infection on expansion of small abdominal aortic aneurysms—A prospective randomized double-blind trial. J. Vasc. Surg. 2009, 50, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Wágsäter, D.; Johansson, D.; Fontaine, V.; Vorkapic, E.; Backlund, A.; Razuvaev, A.; Mayranpaa, M.I.; Hjerpe, C.; Caidahl, K.; Hamsten, A.; et al. Serine protease inhibitor A3 in atherosclerosis and aneurysm disease. Int. J. Mol. Med. 2012, 30, 288–294. [Google Scholar] [PubMed]
- Borst, P.; Grivell, L.A. Mitochondrial ribosomes. FEBS Lett. 1971, 13, 73–88. [Google Scholar] [CrossRef] [PubMed]
- Van den Bogert, C.; Dontje, B.H.; Kroon, A.M. The antitumour effect of doxycycline on a T-cell leukaemia in the rat. Leuk. Res. 1985, 9, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Van den Bogert, C.; Dontje, B.H.; Kroon, A.M. Doxycycline in combination chemotherapy of a rat leukemia. Cancer Res. 1988, 48, 6686–6690. [Google Scholar] [PubMed]
- Amălinei, C.; Căruntu, I.D.; Giuşcă, S.E.; Bălan, R.A. Matrix metalloproteinases involvement in pathologic conditions. Rom. J. Morphol. Embryol. 2010, 51, 215–228. [Google Scholar] [PubMed]
- Remacle, A.; Murphy, G.; Roghi, C. Membrane type 1-matrix metalloproteinase (MT1-MMP) is internalised by two different pathways and is recycled to the cell surface. J. Cell Sci. 2003, 116, 3965–3916. [Google Scholar] [CrossRef]
- Xiong, W.; Knispel, R.; MacTaggart, J.; Greiner, T.C.; Weiss, S.J.; Baxter, B.T. Membrane-type 1 matrix metalloproteinase regulates macrophage-dependent elastolytic activity and aneurysm formation in vivo. J. Biol. Chem. 2009, 284, 1765–1771. [Google Scholar] [CrossRef] [PubMed]
- Vandooren, J.; van den Steen, P.E.; Opdenakker, G. Biochemistry and molecular biology of gelatinase B or matrix metalloproteinase-9 (MMP-9): The next decade. Crit. Rev. Biochem. Mol. Biol. 2013, 48, 222–272. [Google Scholar] [CrossRef] [PubMed]
- Acharya, M.R.; Venitz, J.; Figg, W.D.; Sparreboom, A. Chemically modified tetracyclines as inhibitors of matrix metalloproteinases. Drug Resist. Updates 2004, 7, 195–208. [Google Scholar] [CrossRef]
- Mannello, F.; Tonti, G.; Papa, S. Matrix metalloproteinase inhibitors as anticancer therapeutics. Curr. Cancer Drug Targets 2005, 5, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Gialeli, C.; Theocharis, A.D.; Karamanos, N.K. Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J. 2011, 278, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Lokeshwar, B.L.; Escatel, E.; Zhu, B. Cytotoxic activity and inhibition of tumor cell invasion by derivatives of a chemically modified tetracycline CMT-3 (COL-3). Curr. Med. Chem. 2001, 8, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Tolomeo, M.; Simoni, D. Drug resistance and apoptosis in cancer treatment: Development of new apoptosis-inducing agents active in drug resistant malignancies. Curr. Med. Chem. Anticancer Agents 2002, 2, 387–401. [Google Scholar] [CrossRef] [PubMed]
- Lokeshwar, B.L. Chemically modified non-antimicrobial tetracyclines are multifunctional drugs against advanced cancers. Pharmacol. Res. 2011, 63, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Richards, C.; Pantanowitz, L.; Dezube, B.J. Antimicrobial and non-antimicrobial tetracyclines in human cancer trials. Pharmacol. Res. 2011, 63, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Konstantinopoulos, P.A.; Karamouzis, M.V.; Papatsoris, A.G.; Papavassiliou, A.G. Matrix metalloproteinase inhibitors as anticancer agents. Int. J. Biochem. Cell Biol. 2008, 40, 1156–1168. [Google Scholar] [CrossRef] [PubMed]
- Curci, J.A.; Mao, D.; Bohner, D.G.; Allen, B.T.; Rubin, B.G.; Reilly, J.M.; Sicard, G.A.; Thompson, R.W. Preoperative treatment with doxycycline reduces aortic wall expression and activation of matrix metalloproteinases in patients with abdominal aortic aneurysms. J. Vasc. Surg. 2000, 31, 325–342. [Google Scholar] [CrossRef] [PubMed]
- Prall, A.K.; Longo, G.M.; Mayhan, W.G.; Waltke, E.A.; Fleckten, B.; Thompson, R.W.; Baxter, B.T. Doxycycline in patients with abdominal aortic aneurysms and in mice: Comparison of serum levels and effect on aneurysm growth in mice. J. Vasc. Surg. 2002, 35, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Baxter, B.T. Abdominal aortic aneurysm regression by medical treatment: Possibility or pipe dream? J. Vasc. Surg. 2006, 43, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Xiong, W.; Knispel, R.A.; Dietz, H.C.; Ramirez, F.; Baxter, B.T. Doxycycline delays aneurysm rupture in a mouse model of Marfan syndrome. J. Vasc. Surg. 2008, 47, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Petrinec, D.; Liao, S.; Holmes, D.R.; Reilly, J.M.; Parks, W.C.; Thompson, R.W. Doxycycline inhibition of aneurysmal degeneration in an elastase-induced rat model of abdominal aortic aneurysm: Preservation of aortic elastin associated with suppressed production of 92 kD gelatinase. J. Vasc. Surg. 1996, 23, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.R.; McDermott, E.; Crowther, M.; Wills, A.D.; Bell, P.R.; Thompson, M.M. Doxycycline inhibits elastin degradation and reduces metalloproteinase activity in a model of aneurysmal disease. J. Vasc. Surg. 1998, 27, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Curci, J.A.; Petrinec, D.; Liao, S.; Golub, L.M.; Thompson, R.W. Pharmacologic suppression of experimental abdominal aortic aneurysms: A comparison of doxycycline and four chemically modified tetracyclines. J. Vasc. Surg. 1998, 28, 1082–1093. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.W.; Cassis, L.A.; Daugherty, A. Differential effects of doxycycline, a broad-spectrum matrix metalloproteinase inhibitor, on angiotensin II-induced atherosclerosis and abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Sho, E.; Chu, J.; Sho, M.; Fernandes, B.; Judd, D.; Ganesan, P.; Kimura, H.; Dalman, R.L. Continuous periaortic infusion improves doxycycline efficacy in experimental aortic aneurysms. J. Vasc. Surg. 2004, 39, 1312–1321. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, M.A.; Parodi, F.E.; Chu, J.; Pagano, M.B.; Mao, D.; Baxter, B.T.; Buckley, C.; Ennis, T.L.; Thompson, R.W. Localized administration of doxycycline suppresses aortic dilatation in an experimental mouse model of abdominal aortic aneurysm. Ann. Vasc. Surg. 2006, 20, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Lu, H.; Moorleghen, J.J.; Howatt, D.A.; Rateri, D.L.; Cassis, L.A.; Daugherty, A. Doxycycline does not influence established abdominal aortic aneurisms in angiotensin II-infused mice. PLoS ONE 2012, 7, e46411. [Google Scholar] [CrossRef] [PubMed]
- Sivaraman, B.; Ramamurthi, A. Multifunctional nanoparticles for doxycycline delivery towards localized elastic matrix stabilization and regenerative repair. Acta Biomater. 2013, 9, 6511–6525. [Google Scholar] [CrossRef] [PubMed]
- Bettany, J.T.; Peet, N.M.; Wolowacz, R.G.; Skerry, T.M.; Grabowski, P.S. Tetracyclines induce apoptosis in osteoclasts. Bone 2000, 27, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.W.; Baxter, B.T. MMP inhibition in abdominal aortic aneurysms: Rationale for a prospective randomized clinical trial. Ann. N. Y. Acad. Sci. 1999, 878, 159–178. [Google Scholar] [CrossRef] [PubMed]
- Mosorin, M.; Juvonen, J.; Biancari, F.; Satta, J.; Surcel, H.M.; Leinonen, M.; Saikku, P.; Juvonen, T. Use of doxycycline to decrease the growth rate of abdominal aortic aneurysms: A randomized, double-blind, placebo-controlled pilot study. J. Vasc. Surg. 2001, 34, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Baxter, B.T.; Pearce, W.H.; Waltke, E.A.; Littooy, F.N.; Hallett, J.W., Jr.; Kent, K.C.; Upchurch, G.R., Jr.; Chaikof, E.L.; Mills, J.L.; Fleckten, B.; et al. Prolonged administration of doxycycline in patients with small asymptomatic abdominal aortic aneurysms: Report of a prospective (Phase II) multicenter study. J. Vasc. Surg. 2002, 36, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.L.; Desai, K.K.; Vakili, B.A.; Nouneh, C.; Lee, H.M.; Golub, L.M. Clinical and biochemical results of the metalloproteinase inhibition with subantimicrobial doses of doxycycline to prevent acute coronary syndromes (MIDAS) pilot trial. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Meijer, C.A.; Stijnen, T.; Wasser, M.N.J.M.; Hamming, J.F.; van Bockel, J.H.; Lindeman, J.H.N. Doxycycline for stabilization of abdominal aortic aneurysms: A randomized trial. Ann. Intern. Med. 2013, 159, 815–823. [Google Scholar] [PubMed]
- ClinicalTrails.gov Identifier: NCT01756833. Available online: https://www.clinicaltrails.gov/show/NCT01756833 (accessed on 27 November 2014).
- Gu, Y.; Walker, C.; Ryan, M.E.; Payne, J.B.; Golub, L.M. Non-antibacterial tetracycline formulations: Clinical applications in dentistry and medicine. J. Oral Microbiol. 2012, 4, 19227. [Google Scholar] [CrossRef]
- Cunha, B.A.; Comer, J.B.; Jonas, M. The tetracyclines. Med. Clin. N. Am. 1982, 66, 293–302. [Google Scholar] [PubMed]
- Welling, P.G.; Koch, P.A.; Lau, C.C.; Craig, W.A. Bioavailability of tetracycline and doxycycline in fasted and nonfasted subjects. Antimicrob. Agents Chemother. 1977, 11, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Van den Bogert, C.; van Kernebeek, G.; de Leij, L.; Kroon, A.M. Inhibition of mitochondrial protein synthesis leads to proliferation arrest in the G1-phase of the cell cycle. Cancer Lett. 1986, 32, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Ogrinc, K.; Logar, M.; Lotrič-Furlan, S.; Cerar, D.; Ružić-Sabljic, E.; Strle, F. Doxycycline versus ceftriaxone for the treatment of patients with chronic Lyme borreliosis. Wien. Klin. Wochenschr. 2006, 118, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Ljøstad, U.; Skogvoll, E.; Eikeland, R.; Midgard, R.; Skarpaas, T.; Berg, A.; Mygland, A. Oral doxycycline versus intravenous ceftriaxone for European Lyme neuroborreliosis: A multicentre, non-inferiority, double-blind, randomised trial. Lancet Neurol. 2008, 7, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Borg, R.; Dotevall, L.; Hagberg, L.; Maraspin, V.; Lotric-Furlan, S.; Cimperman, J.; Strle, F. Intravenous ceftriaxone compared with oral doxycycline for the treatment of Lyme neuroborreliosis. Scand. J. Infect. Dis. 2005, 37, 449–454. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kroon, A.M.; Taanman, J.-W. Clonal Expansion of T Cells in Abdominal Aortic Aneurysm: A Role for Doxycycline as Drug of Choice? Int. J. Mol. Sci. 2015, 16, 11178-11195. https://doi.org/10.3390/ijms160511178
Kroon AM, Taanman J-W. Clonal Expansion of T Cells in Abdominal Aortic Aneurysm: A Role for Doxycycline as Drug of Choice? International Journal of Molecular Sciences. 2015; 16(5):11178-11195. https://doi.org/10.3390/ijms160511178
Chicago/Turabian StyleKroon, Albert M., and Jan-Willem Taanman. 2015. "Clonal Expansion of T Cells in Abdominal Aortic Aneurysm: A Role for Doxycycline as Drug of Choice?" International Journal of Molecular Sciences 16, no. 5: 11178-11195. https://doi.org/10.3390/ijms160511178