Development of Triamcinolone Acetonide-Loaded Nanostructured Lipid Carriers (NLCs) for Buccal Drug Delivery Using the Box-Behnken Design
Abstract
:1. Introduction
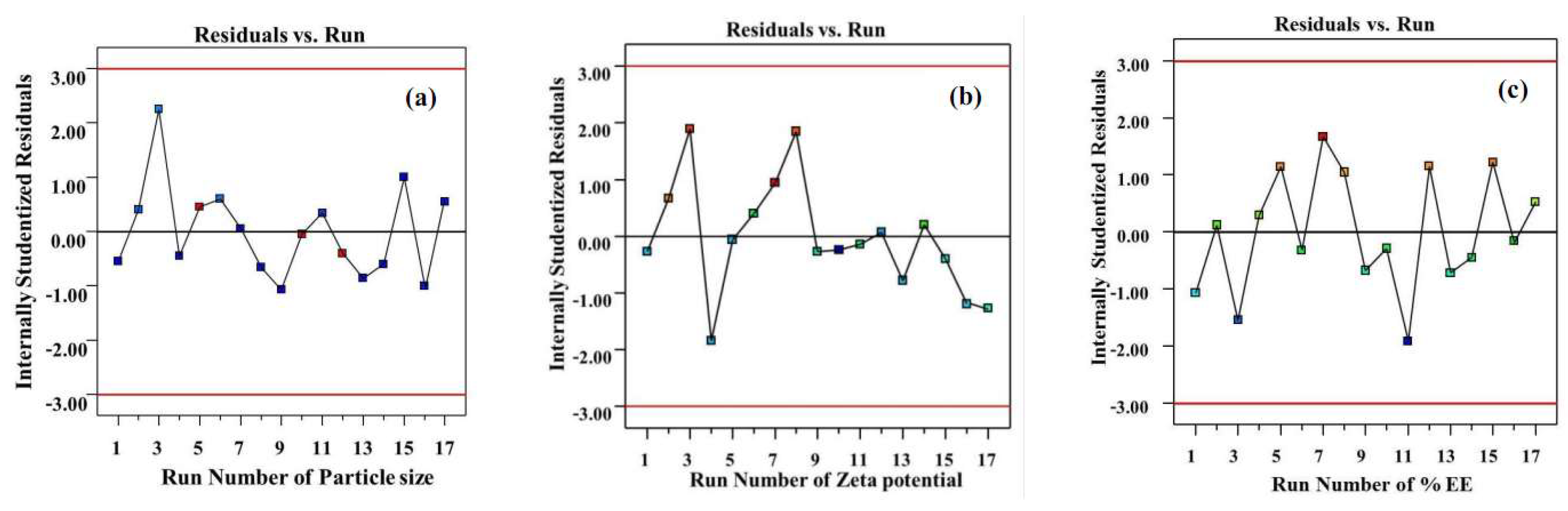
2. Results and Discussion
2.1. Physicochemical Characterization of TA Loaded NLC (Zeta Potential and Particle Size)
2.2. Determination of Entrapment Efficiency
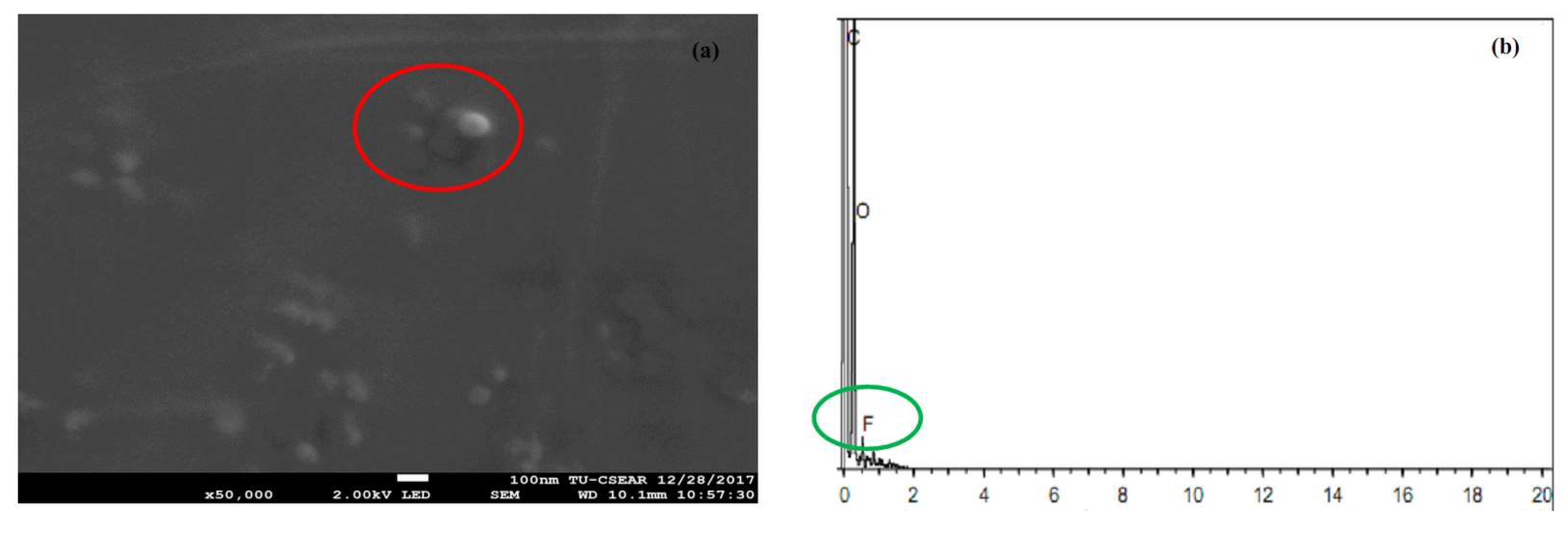
2.3. Field Emission Scanning Electron Microscope (FESEM) and Energy-Dispersive X-ray Spectroscopy (EDS)
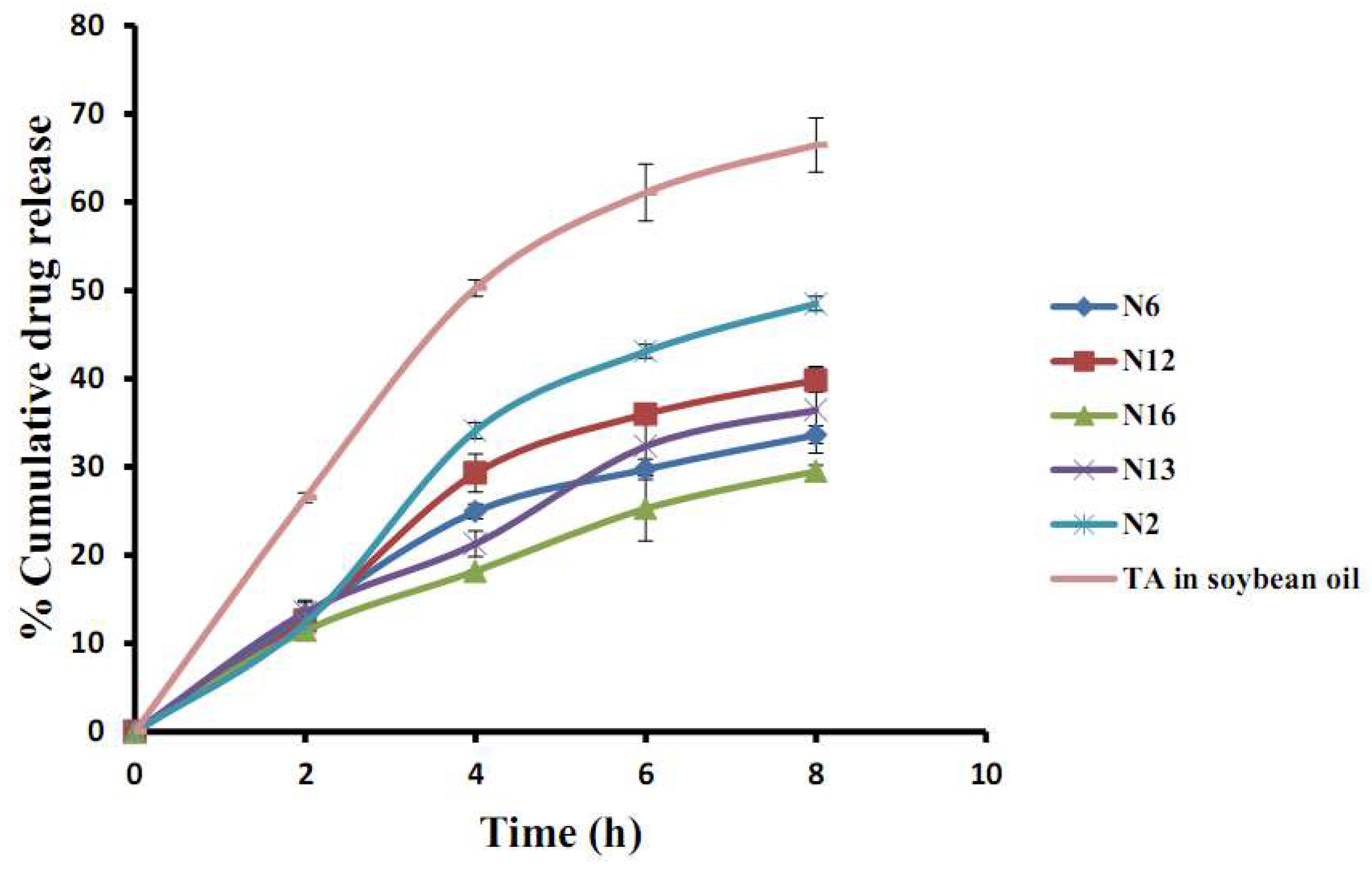
2.4. In Vitro Release of TA Loaded NLC
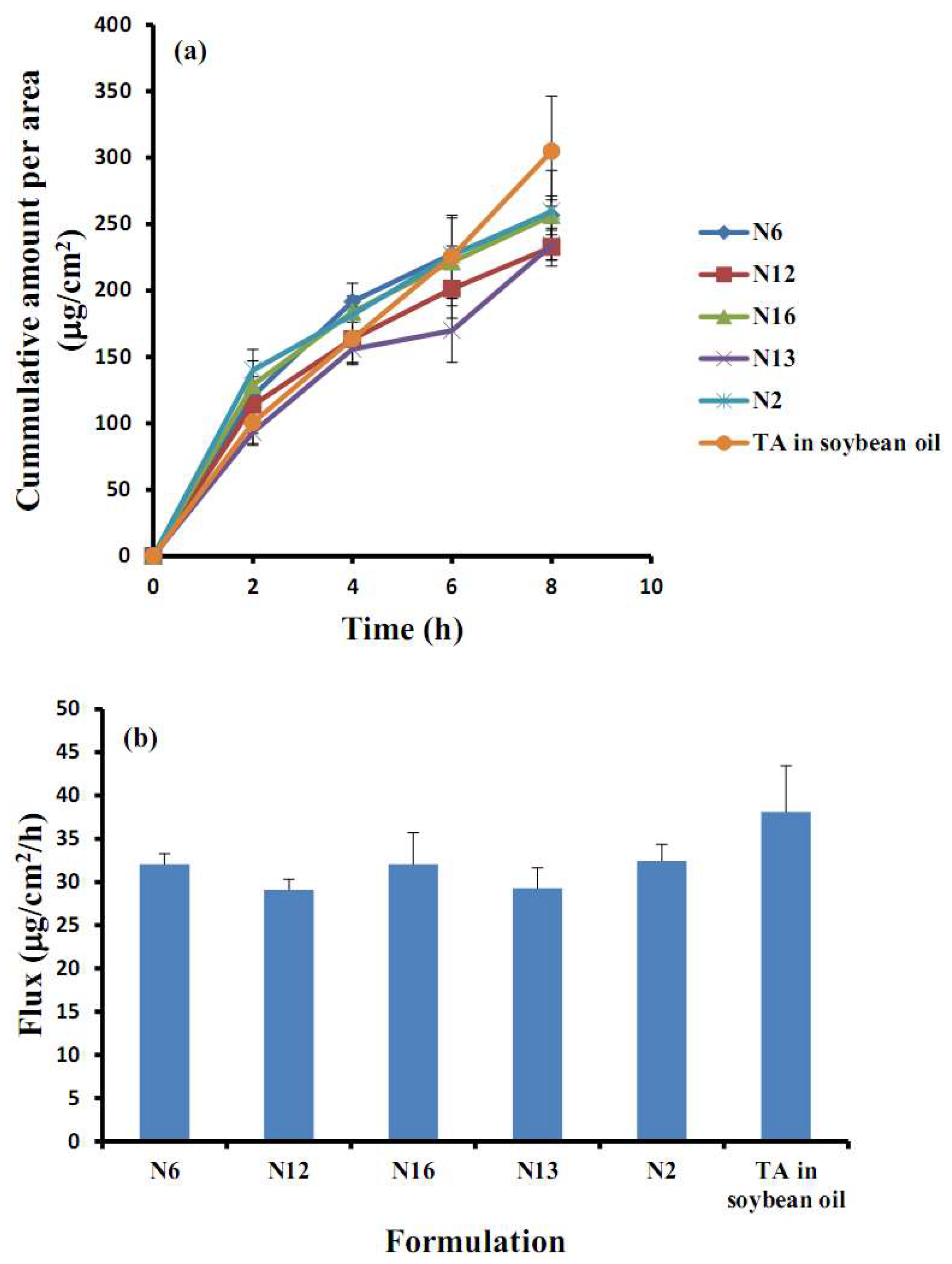
2.5. In Vitro Permeation Studies
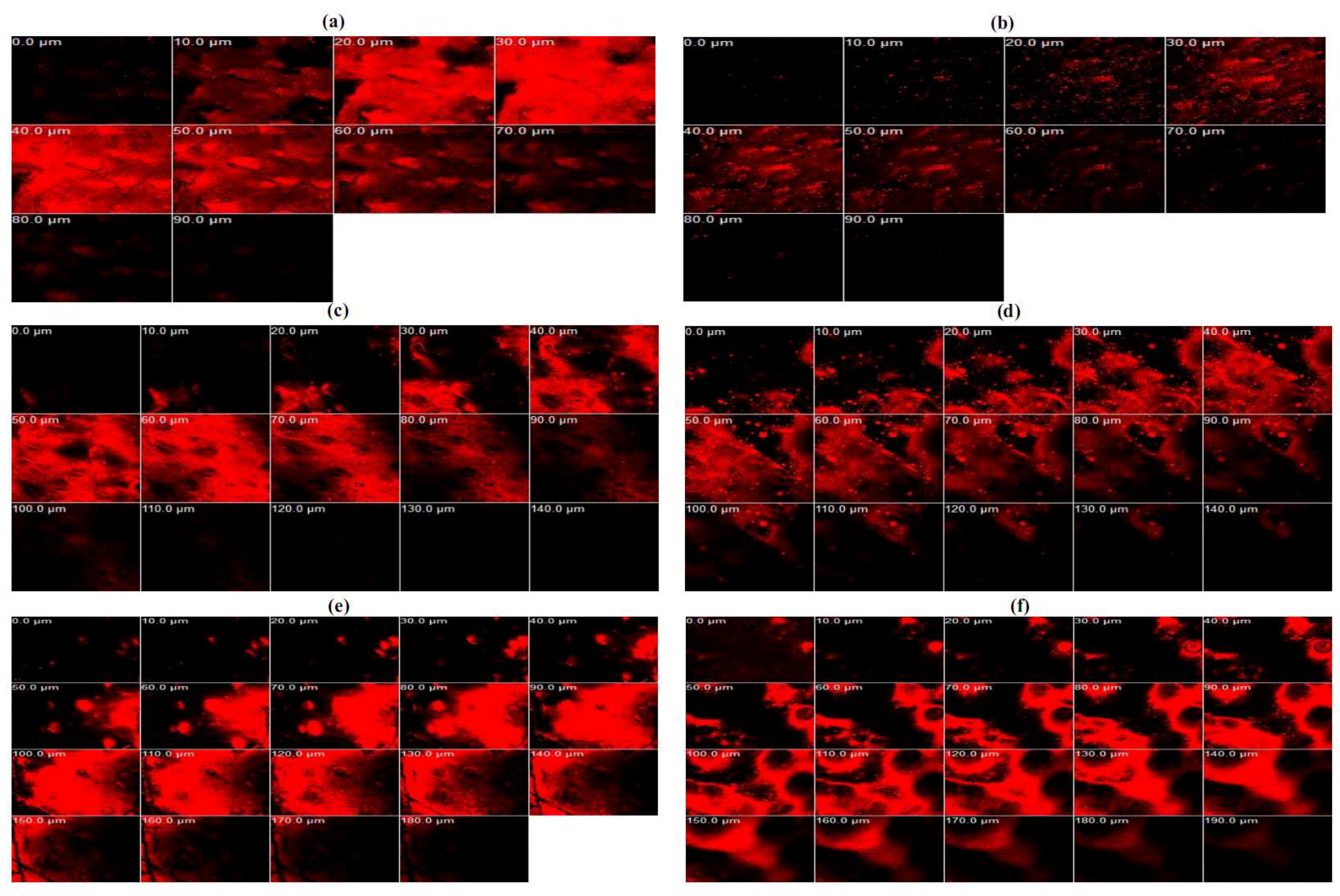
2.6. Confocal Laser Scanning Microscopy (CLSM) Study
3. Materials and Methods
3.1. Materials
3.2. Preparation of TA Loaded NLC
3.3. Experimental Design and Statistical Analysis
3.4. Physicochemical Characterization of TA Loaded NLC (Zeta Potential and Particle Size)
3.5. Determination of Entrapment Efficiency
3.6. Field Emission Scanning Electron Microscope (FESEM) and Energy-Dispersive X-ray Spectroscopy (EDS)
3.7. In Vitro Release of TA-Loaded NLCs
3.8. In Vitro Permeation Studies
3.9. Confocal Laser Scanning Microscopy (CLSM) Study
3.10. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Funding
Conflicts of Interest
References
- Shin, S.-C.; Kim, J.-Y. Enhanced permeation of triamcinolone acetonide through the buccal mucosa. Eur. J. Pharm. Biopharm. 2000, 50, 217–220. [Google Scholar] [CrossRef]
- Kraisit, P.; Limmatvapirat, S.; Luangtana-Anan, M.; Sriamornsak, P. Buccal administration of mucoadhesive blend films saturated with propranolol loaded nanoparticles. Asian J. Pharm. Sci. 2018, 13, 34–43. [Google Scholar] [CrossRef]
- Tetyczka, C.; Griesbacher, M.; Absenger-Novak, M.; Fröhlich, E.; Roblegg, E. Development of nanostructured lipid carriers for intraoral delivery of domperidone. Int. J. Pharm. 2017, 526, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Morales, J.O.; McConville, J.T. Manufacture and characterization of mucoadhesive buccal films. Eur. J. Pharm. Biopharm. 2011, 77, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Morales, J.O.; McConville, J.T. Novel strategies for the buccal delivery of macromolecules. Drug Dev. Ind. Pharm. 2014, 40, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, M.; Singh, D.; Singh, M.R. Fabrication, optimization and characterization of triamcinolone acetonide loaded nanostructured lipid carriers for topical treatment of psoriasis: Application of box behnken design, in vitro and ex vivo studies. J. Drug Deliv. Sci. Technol. 2017, 41, 325–333. [Google Scholar] [CrossRef]
- Fang, C.L.; Al-Suwayeh, S.A.; Fang, J.Y. Nanostructured lipid carriers (nlcs) for drug delivery and targeting. Recent Pat. Nanotechnol. 2013, 7, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Araújo, J.; Nikolic, S.; Egea, M.A.; Souto, E.B.; Garcia, M.L. Nanostructured lipid carriers for triamcinolone acetonide delivery to the posterior segment of the eye. Colloids Surf. B Biointerfaces 2011, 88, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Moghddam, S.M.M.; Ahad, A.; Aqil, M.; Imam, S.S.; Sultana, Y. Optimization of nanostructured lipid carriers for topical delivery of nimesulide using box–behnken design approach. Artif. Cells Nanomed. Biotechnol. 2017, 45, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Pardeike, J.; Hommoss, A.; Müller, R.H. Lipid nanoparticles (sln, nlc) in cosmetic and pharmaceutical dermal products. Int. J. Pharm. 2009, 366, 170–184. [Google Scholar] [CrossRef] [PubMed]
- Tamjidi, F.; Shahedi, M.; Varshosaz, J.; Nasirpour, A. Nanostructured lipid carriers (nlc): A potential delivery system for bioactive food molecules. Innov. Food Sci. Emerg. Technol. 2013, 19, 29–43. [Google Scholar] [CrossRef]
- Teeranachaideekul, V.; Boonme, P.; Souto, E.B.; Müller, R.H.; Junyaprasert, V.B. Influence of oil content on physicochemical properties and skin distribution of nile red-loaded nlc. J. Control. Release 2008, 128, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.-O.; Choe, J.; Suh, S.; Ko, S. Positively charged nanostructured lipid carriers and their effect on the dissolution of poorly soluble drugs. Molecules 2016, 21. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, L.N.M.; Breitkreitz, M.C.; Guilherme, V.A.; da Silva, G.H.R.; Couto, V.M.; Castro, S.R.; de Paula, B.O.; Machado, D.; de Paula, E. Natural lipids-based nlc containing lidocaine: From pre-formulation to in vivo studies. Eur. J. Pharm. Sci. 2017, 106, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Li, D.; Luo, Y.-F.; He, X.-J.; Jiang, M.-Y. Preparation and in vitro evaluation of glycyrrhetinic acid-modified curcumin-loaded nanostructured lipid carriers. Molecules 2014, 19, 2445–2457. [Google Scholar] [CrossRef] [PubMed]
- Kovacevic, A.; Savic, S.; Vuleta, G.; Müller, R.H.; Keck, C.M. Polyhydroxy surfactants for the formulation of lipid nanoparticles (sln and nlc): Effects on size, physical stability and particle matrix structure. Int. J. Pharm. 2011, 406, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Esposito, E.; Ravani, L.; Drechsler, M.; Mariani, P.; Contado, C.; Ruokolainen, J.; Ratano, P.; Campolongo, P.; Trezza, V.; Nastruzzi, C.; et al. Cannabinoid antagonist in nanostructured lipid carriers (nlcs): Design, characterization and in vivo study. Mater. Sci. Eng. C 2015, 48, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Jafari, S.; Maleki-Dizaji, N.; Barar, J.; Barzegar-Jalali, M.; Rameshrad, M.; Adibkia, K. Physicochemical characterization and in vivo evaluation of triamcinolone acetonide-loaded hydroxyapatite nanocomposites for treatment of rheumatoid arthritis. Colloids Surf. B Biointerfaces 2016, 140, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Nicolazzo, J.A.; Reed, B.L.; Finnin, B.C. Enhancing the buccal mucosal uptake and retention of triamcinolone acetonide. J. Control. Release 2005, 105, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, A.; Davaran, S.; Fayyazi, B.; Tanhaei, A.; Payab, S.; Adibkia, K. Application of electrospraying as a one-step method for the fabrication of triamcinolone acetonide-plga nanofibers and nanobeads. Colloids Surf. B Biointerfaces 2014, 123, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Kraisit, P.; Limmatvapirat, S.; Nunthanid, J.; Sriamornsak, P.; Luangtana-Anan, M. Preparation and characterization of hydroxypropyl methylcellulose/polycarbophil mucoadhesive blend films using a mixture design approach. Chem. Pharm. Bull. 2017, 65, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.; Jain, K.; Gowthamarajan, K. Optimization of curcumin nanoemulsion for intranasal delivery using design of experiment and its toxicity assessment. Colloids Surf. B Biointerfaces 2014, 113, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Rahman, Z.; Zidan, A.S.; Khan, M.A. Non-destructive methods of characterization of risperidone solid lipid nanoparticles. Eur. J. Pharm. Biopharm. 2010, 76, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, H.; Kohli, K.; Amin, S.; Rathee, P.; Kumar, V. Optimization and formulation design of gels of diclofenac and curcumin for transdermal drug delivery by box-behnken statistical design. J. Pharm. Sci. 2011, 100, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Mehta, S.K. Developments of polysorbate (tween) based microemulsions: Preclinical drug delivery, toxicity and antimicrobial applications. Int. J. Pharm. 2017, 529, 134–160. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhao, L.; Almasy, L.; Garamus, V.M.; Zou, A.; Willumeit, R.; Fan, S. Preparation and characterization of 4-dedimethylamino sancycline (cmt-3) loaded nanostructured lipid carrier (cmt-3/nlc) formulations. Int. J. Pharm. 2013, 450, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Kraisit, P.; Limmatvapirat, S.; Nunthanid, J.; Sriamornsak, P.; Luangtana-anan, M. Nanoparticle formation by using shellac and chitosan for a protein delivery system. Pharm. Dev. Technol. 2013, 18, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Nanostructured lipid matrices for improved microencapsulation of drugs. Int. J. Pharm. 2002, 242, 121–128. [Google Scholar] [CrossRef]
- Higuchi, T. Mechanism of sustained-action medication. Theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J. Pharm. Sci. 1963, 52, 1145–1149. [Google Scholar] [CrossRef] [PubMed]
- Zhigaltsev, I.V.; Winters, G.; Srinivasulu, M.; Crawford, J.; Wong, M.; Amankwa, L.; Waterhouse, D.; Masin, D.; Webb, M.; Harasym, N.; et al. Development of a weak-base docetaxel derivative that can be loaded into lipid nanoparticles. J. Control. Release 2010, 144, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Shalel, S.; Streichman, S.; Marmur, A. Monitoring surfactant-induced hemolysis by surface tension measurement. J. Colloid Interface Sci. 2002, 255, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Subongkot, T.; Ngawhirunpat, T. Development of a novel microemulsion for oral absorption enhancement of all-trans retinoic acid. Int. J. Nanomed. 2017, 12, 5585–5599. [Google Scholar] [CrossRef] [PubMed]
- Salamat-Miller, N.; Chittchang, M.; Johnston, T.P. The use of mucoadhesive polymers in buccal drug delivery. Adv. Drug Deliv. Rev. 2005, 57, 1666–1691. [Google Scholar] [CrossRef] [PubMed]
Sample Availability: Samples of the compounds are not available from the authors. |



| Formulation | Actual Value of Independent Factors | Response Values | ||||
|---|---|---|---|---|---|---|
| Spermaceti (g), X1 | Soybean Oil (g), X2 | Tween 80 (g), X3 | Particle Size (nm), Y1 | Zeta Potential (mV), Y2 | EE (%), Y3 | |
| N1 | 1.0 | 0.25 | 3.0 | 80.75 | −17.91 | 86.89 |
| N2 | 1.0 | 0.50 | 4.0 | 81.15 | −17.98 | 93.96 |
| N3 | 1.0 | 0.50 | 2.0 | 93.35 | −14.49 | 90.77 |
| N4 | 1.0 | 0.75 | 3.0 | 91.60 | −8.16 | 93.07 |
| N5 | 1.5 | 0.25 | 2.0 | 185.20 | −20.83 | 90.94 |
| N6 | 1.5 | 0.25 | 4.0 | 80.50 | −17.07 | 98.76 |
| N7 | 1.5 | 0.50 | 3.0 | 95.10 | −6.90 | 84.45 |
| N8 | 1.5 | 0.50 | 3.0 | 82.70 | −7.09 | 97.84 |
| N9 | 1.5 | 0.50 | 3.0 | 80.95 | −15.7 | 88.95 |
| N10 | 1.5 | 0.50 | 3.0 | 86.95 | −15.18 | 82.52 |
| N11 | 1.5 | 0.50 | 3.0 | 81.85 | −17.77 | 88.72 |
| N12 | 1.5 | 0.75 | 4.0 | 82.15 | −5.91 | 101.09 |
| N13 | 1.5 | 0.75 | 2.0 | 83.15 | −17.67 | 91.61 |
| N14 | 2.0 | 0.25 | 3.0 | 184.75 | −18.47 | 98.40 |
| N15 | 2.0 | 0.50 | 2.0 | 185.80 | −17.83 | 98.36 |
| N16 | 2.0 | 0.50 | 4.0 | 82.25 | −12.60 | 90.10 |
| N17 | 2.0 | 0.75 | 3.0 | 82.55 | −16.64 | 95.14 |
| Mathematical Release Models | N6 (R2) | N12 (R2) | N16 (R2) | N13 (R2) | N2 (R2) |
|---|---|---|---|---|---|
| Zero-order | 0.9351 | 0.942 | 0.9715 | 0.9736 | 0.9522 |
| First-order | 0.8572 | 0.8153 | 0.9547 | 0.9481 | 0.8073 |
| Higuchi | 0.9823 | 0.9561 | 0.9812 | 0.967 | 0.9329 |
| Independent Factors | Levels | ||
|---|---|---|---|
| −1 | 0 | +1 | |
| Spermaceti (g), X1 | 1.0 | 1.5 | 2.0 |
| Soybean oil (g), X2 | 0.25 | 0.50 | 0.75 |
| Tween 80 (g), X3 | 2.0 | 3.0 | 4.0 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kraisit, P.; Sarisuta, N. Development of Triamcinolone Acetonide-Loaded Nanostructured Lipid Carriers (NLCs) for Buccal Drug Delivery Using the Box-Behnken Design. Molecules 2018, 23, 982. https://doi.org/10.3390/molecules23040982
Kraisit P, Sarisuta N. Development of Triamcinolone Acetonide-Loaded Nanostructured Lipid Carriers (NLCs) for Buccal Drug Delivery Using the Box-Behnken Design. Molecules. 2018; 23(4):982. https://doi.org/10.3390/molecules23040982
Chicago/Turabian StyleKraisit, Pakorn, and Narong Sarisuta. 2018. "Development of Triamcinolone Acetonide-Loaded Nanostructured Lipid Carriers (NLCs) for Buccal Drug Delivery Using the Box-Behnken Design" Molecules 23, no. 4: 982. https://doi.org/10.3390/molecules23040982






