LC-UV Determination of Baicalin in Rabbit Plasma and Tissues for Application in Pharmacokinetics and Tissue Distribution Studies of Baicalin after Intravenous Administration of Liposomal and Injectable Formulations
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characteristics of Baicalin Loaded Liposomes
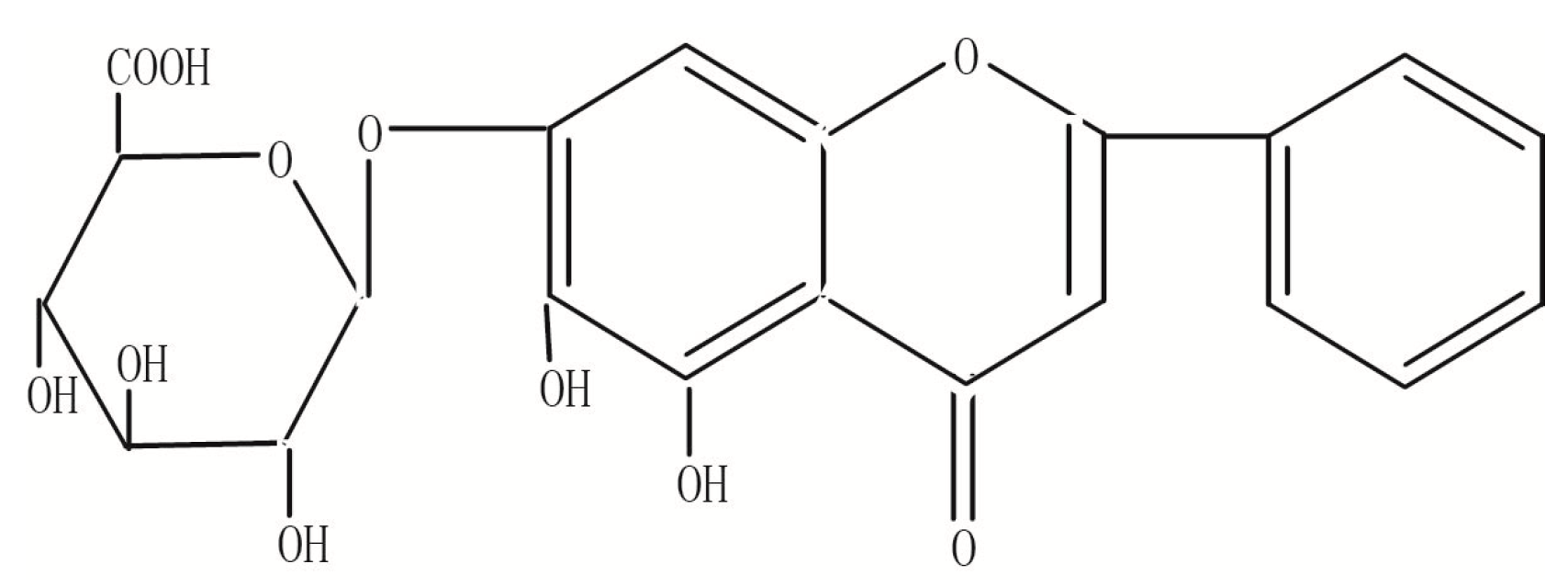
2.2. Optimization of Chromatographic Condition
2.3. Assay Validation
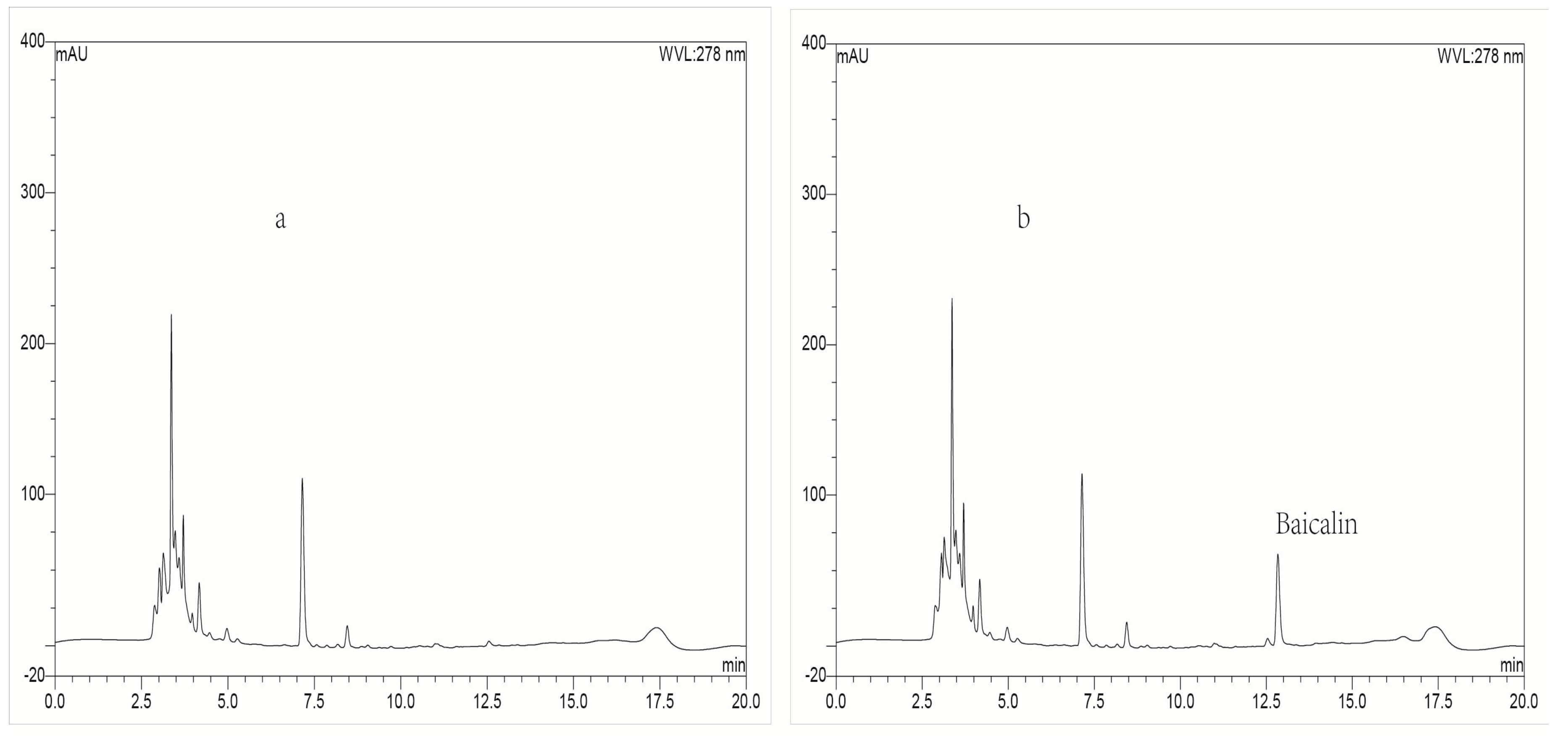
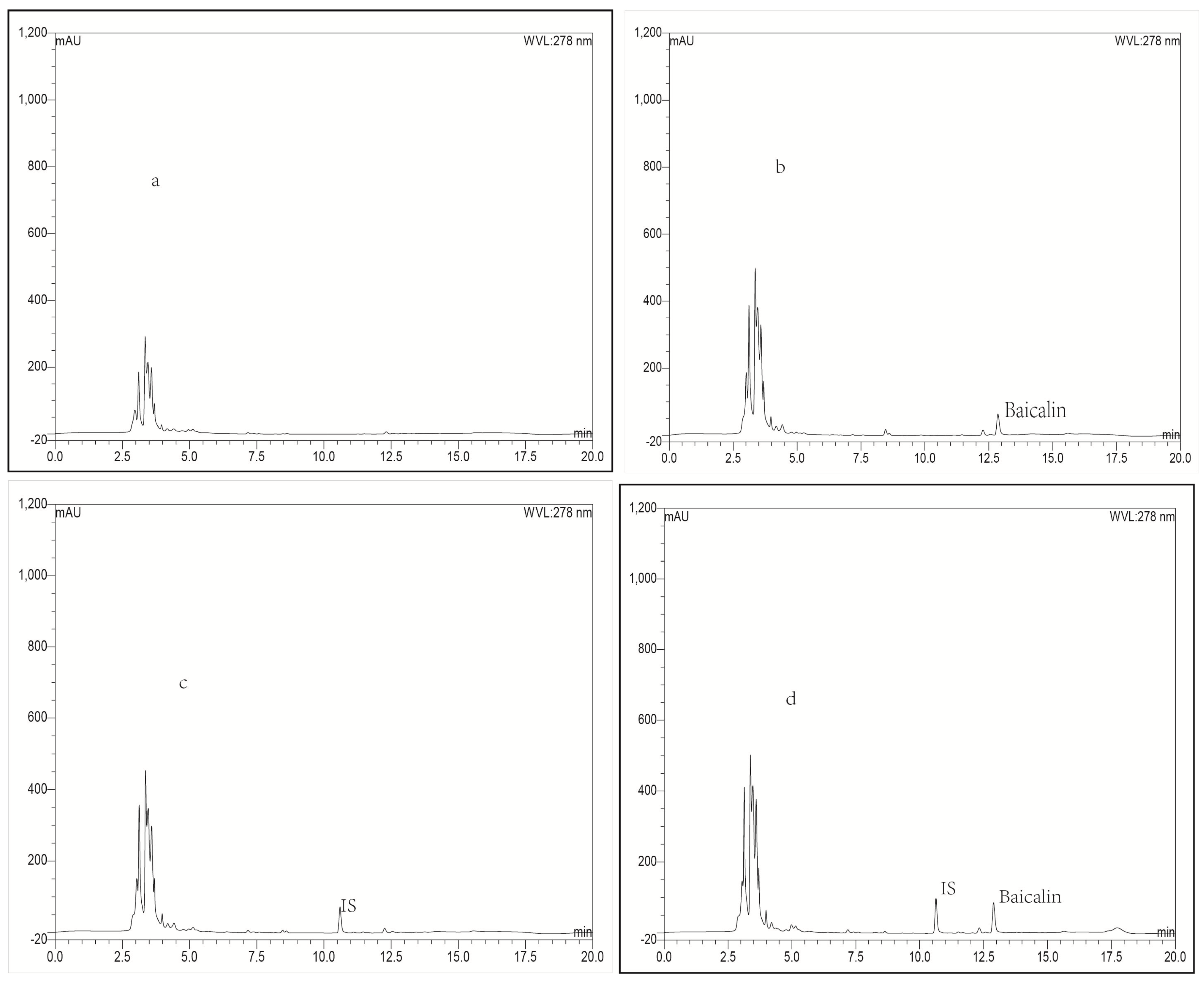
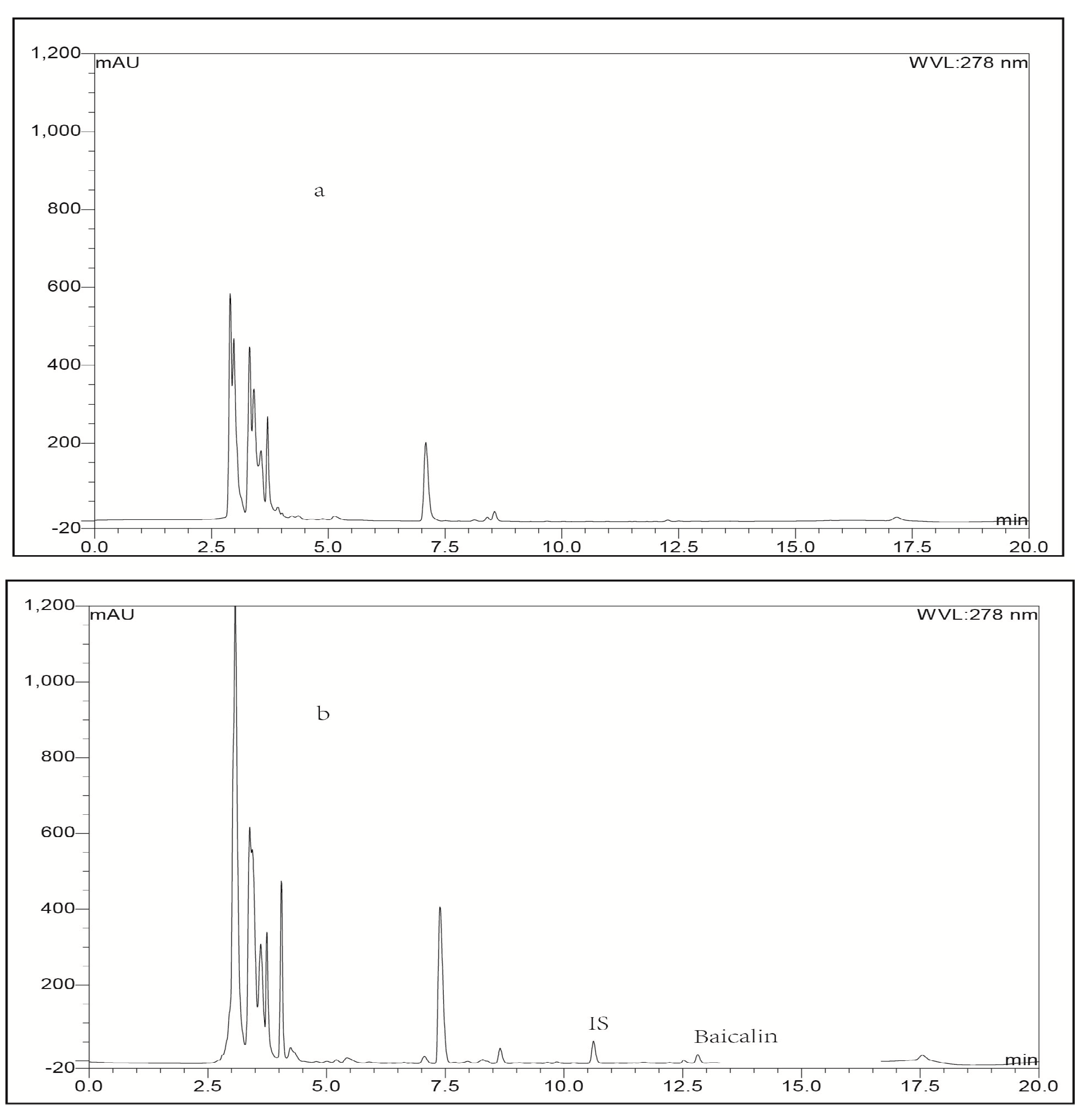
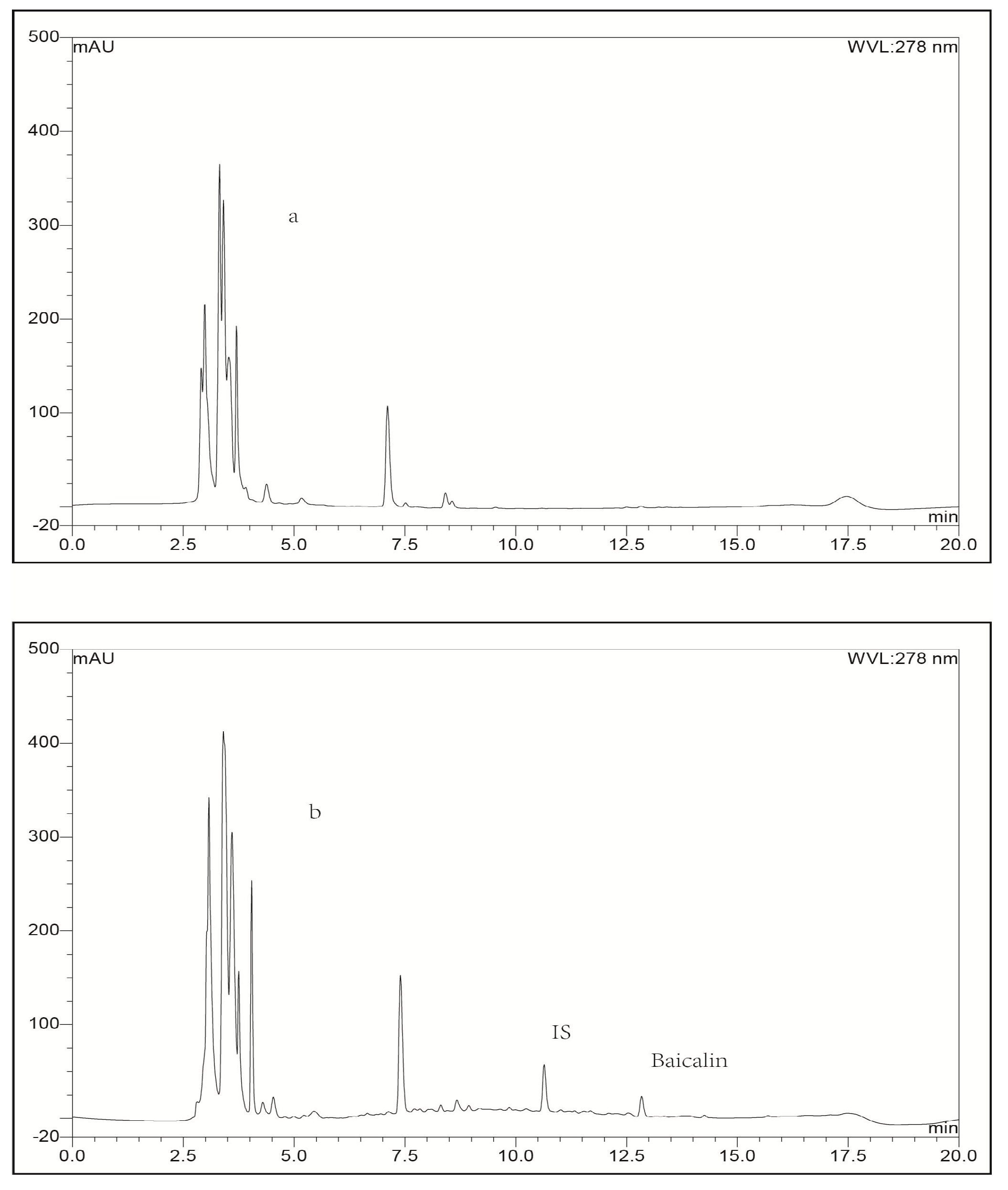
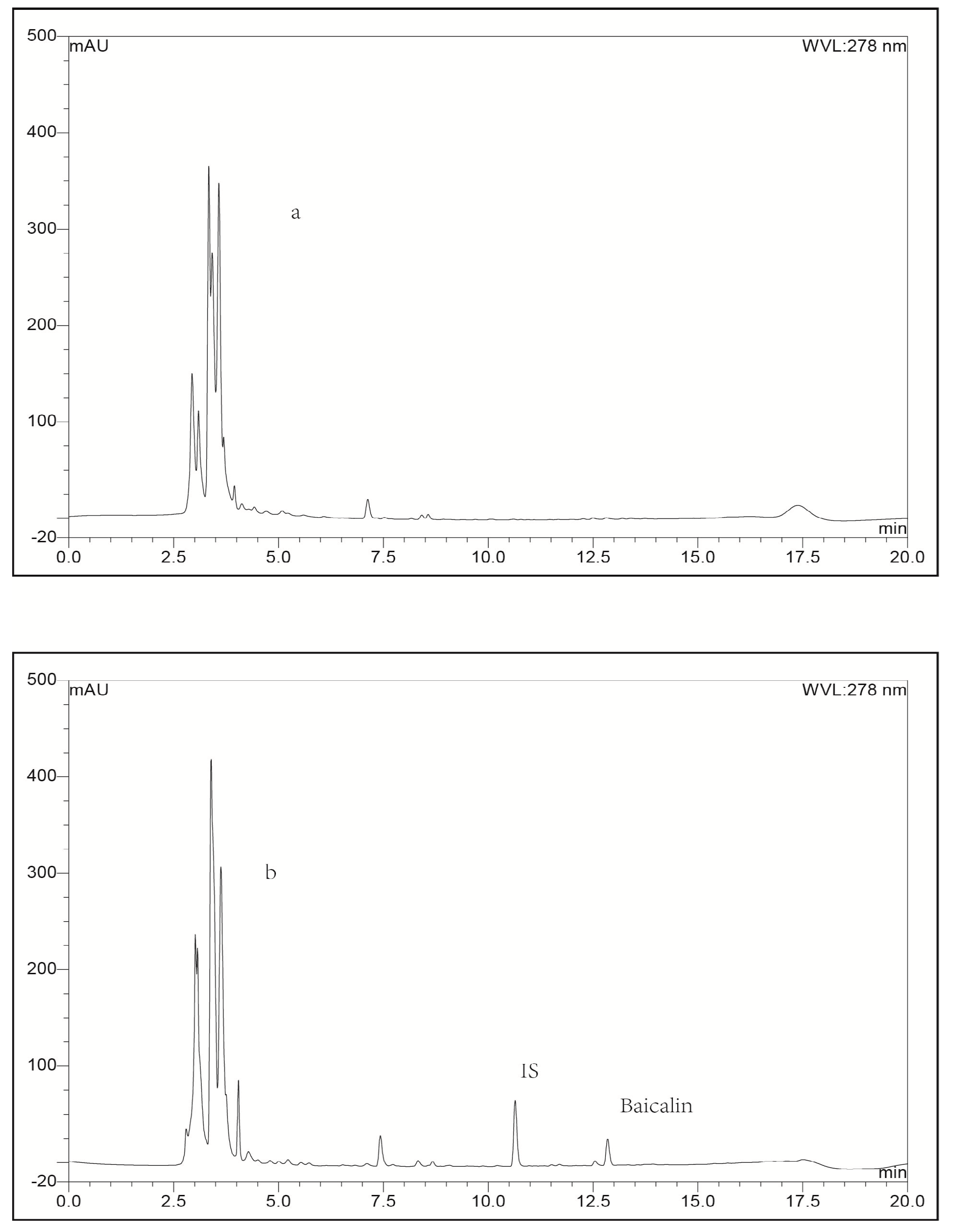
2.3.1. Selectivity
2.3.2. Linearity Range, Limit of Quantification and Limit of Detection
2.3.3. Accuracy and Precision
2.3.4. Extraction Recovery
2.3.5. Stability
2.4. Pharmacokinetics and Tissue Distribution Study
2.4.1. Plasma Pharmacokinetics Study
2.4.2. Tissue Distribution Study
3. Materials and Methods
3.1. Materials and Animals
3.2. Preparation of Baicalin Lposomes
3.3. Equipment and LC-UV Conditions
3.4. Preparation of Calibration Standards and Quality Control Samples
3.5. Validation of Analysis Method
3.6. Application in Pharmacokinetics and Tissue Distribution Study
3.7. Data Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Pan, T.L.; Wang, P.W.; Huang, C.H.; Leu, Y.L.; Wu, T.H.; Wu, Y.R.; You, J.S. Herbal formula, Scutella-riae radix and Rhei rhizoma attenuate dimethylnitrosamine-induced liver fibrosis in a rat model. Sci. Rep. 2015, 5, 11734–11741. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Feng, L.; Zhang, Z.H.; Jia, X.B. The anti-inflammation effect of baicalin on experimental colitis through inhibiting TLR4/NF-κB pathway activation. Int. Immunopharmacol. 2014, 23, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.C.; Chen, S.F.; Lee, Y.M.; Chuang, C.L.; Bau, D.T.; Lin, S.S. Baicalin scavenges reactive oxygen species and protects human keratinocytes against UVC-induced cytotoxicity. Vivo 2013, 27, 707–714. [Google Scholar]
- Lixuan, Z.; Jingcheng, D.; Wenqin, Y.; Jianhua, H.; Baojun, L.; Xiaotao, F. Baicalin attenuates inflammation by inhibiting NF-κB activation in cigarette smoke induced inflammatory models. Pulm. Pharmacol. Ther. 2010, 23, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Chan, F.L.; Choi, H.L.; Chen, Z.Y.; Chan, P.S.; Huang, Y. Induction of apoptosis in prostate cancer cell lines by a flavonoid, baicalin. Cancer Lett. 2000, 160, 219–228. [Google Scholar] [CrossRef]
- Srinivas, N.R. Baicalin, an emerging multi-therapeutic agent: Pharmacodynamics, pharmacokinetics, and considerations from drug development perspectives. Xenobiotica 2010, 40, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, M.; Chao, J.; Shuang, S. Preparation and characterization of the inclusion complex of Baicalin (BG) with beta-CD and HP-β-CD in solution: An antioxidant ability study. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2009, 73, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Wei, Y.; Huang, Y.; He, B.; Zhou, Y.; Fu, J. Nanoemulsion improves the oral bioavailability of baicalin in rats: In vitro and in vivo evaluation. Int. J. Nanomed. 2013, 8, 3769–3779. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, L.; He, Q.; Liu, X.; Okeke, C.I.; Tong, L.; Guo, L.; Yang, H.; Zhang, Q.; Zhao, H.; et al. Effect of Baicalin-loaded PEGylated cationic solid lipid nanoparticles modified by OX26 antibody on regulating the levels of baicalin and amino acids during cerebral ischemia-reperfusion in rats. Int. J. Pharm. 2015, 489, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Je, Y.J.; Yang, M.; Jiang, X.H.; Ma, J.H. Pharmacokinetics of baicalin-phospholipid complex in rat plasma and brain tissues after intranasal and intravenous administration. Pharmazie 2011, 66, 374–377. [Google Scholar] [PubMed]
- Wu, J.; Chen, D.; Zhang, R. Study on the bioavailability of baicalin-phospholipid complex by using HPLC. Biomed. Chromatogr. 1999, 13, 493–495. [Google Scholar] [CrossRef]
- Li, B.; He, M.; Li, W.; Luo, Z.; Guo, Y.; Li, Y.; Zang, C.; Wang, B.; Li, F.; Li, S.; et al. Dissolution and pharmacokinetics of baicalin-polyvinylpyrrolidone coprecipitate. J. Pharm. Pharmacol. 2013, 65, 1670–1678. [Google Scholar] [CrossRef] [PubMed]
- Du, G.; Han, G.; Zhang, S.; Lin, H.; Wu, X.; Wang, M.; Ji, L.; Lu, L.; Yu, L.; Liang, W. Baicalin sup-presses lung carcinoma and lung metastasis by SOD mimic and HIF-1alpha inhibition. Eur. J. Pharmacol. 2010, 630, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xia, X.; Zhang, S.; Zhang, A.; Bo, W.; Zhou, R. Up-regulation of Toll-like receptor 4 was suppressed by emodin and baicalin in the setting of acute pancreatitis. Biomed. Pharmacother. 2009, 63, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Xiong, Y.; Chen, N.; Wang, D.; Lai, Y.; Deng, C. Highly selective enrichment of baicalin in rat plasma by boronic acid-functionalized core-shell magnetic microspheres: Validation and application to a pharmacokinetic study. Talanta 2016, 147, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.M.; Lin, L.C.; Tsai, T.H. Determination and pharmacokinetic study of gentiopicroside, geniposide, baicalin, and swertiamarin in Chinese herbal formulae after oral administration in rats by LC-MS/MS. Molecules 2014, 19, 21560–21578. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, Z.; Li, Y.J.; Wu, X.W.; Wang, S.R.; Chen, K.; Zheng, X.X.; Du, Q.; Tang, D.Q. Simultaneous determination of baicalin, oroxylin A-7-O-glucuronide and wogonoside in rat plasma by UPLC-DAD and its application in pharmacokinetics of pure baicalin, Radix Scutellariae and Yinhuang granule. Biomed. Chromatogr. 2015, 29, 1819–1825. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.B.; Qian, X.C.; Huang, P.; Zhang, Y.X.; Li, J.S.; Yang, G.M.; Cai, B.C. Simultaneous determination of ten flavonoids of crude and wine-processed Radix Scutellariae aqueous extracts in rat plasma by UPLC-ESI-MS/MS and its application to a comparative pharmacokinetic study. Biomed. Chromatogr. 2015, 29, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Shan, W.; Cheng, J.; Qu, B.; Sai, J.; Kong, H.; Qu, H.; Zhao, Y.; Wang, Q. Development of a Fluorescence-Linked Immunosorbent Assay for Baicalin. J. Fluoresc. 2015, 25, 1371–1376. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; He, W.; Li, D.; He, L.; Zhang, W. Preparation and in vitro Anti-tumor Effect of Baicalin Liposome. China J. Exp. Tradit. Med. Formula 2012, 18, 29–31. [Google Scholar]
- Chen, Y.J.; Jia, Y.; Jin, R.; Xu, J.Y.; Xing, X.; Yuan, J.L.; Liu, S.Z. Preparation of Baicalin Flexible nano Liposomes. China J. Exp. Tradit. Med. Formula 2011, 17, 1–4. [Google Scholar]
- Li, T.; Zhang, L.; Tong, L.; Liao, Q. High-throughput salting-out-assisted homogeneous liquid-liquid extraction with acetonitrile for determination of baicalin in rat plasma with high-performance liquid chromatography. Biomed. Chromatogr. 2014, 28, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Gao, R.; Zheng, Q.; Gong, T.; Fu, Y.; Deng, L.; Zhang, Z.R. Gradient high-performance liquid chromatography for the simultaneous determination of chlorogenic acid and baicalin in plasma and its application in the study of pharmacokinetics in rats. J. Pharm. Biomed. Anal. 2007, 43, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Qiu, F.; He, Z.G.; Li, H.Z. HPLC analyses and pharmacokinetic studies of baicalin and oxymat-rine in rabbits. Pharmazie 2003, 58, 616–619. [Google Scholar]
- Xing, J.; Chen, X.; Zhong, D. Stability of baicalin in biological fluids in vitro. J. Pharm. Biomed. Anal. 2005, 39, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.Q.; Han, J.; Xie, Z.Y.; Liao, Q.F.; Zhang, L. Determination of plasma protein binding rate of multicomponent in S cutellaria baicalensis Georgi. Chin. Pharmacol. Bull. 2012, 28, 286–289. [Google Scholar]
- Kim, Y.H.; Jeong, D.W.; Paek, I.B.; Ji, H.Y.; Kim, Y.C.; Sohn, D.H.; Lee, H.S. Liquid chrom-atography with tandem mass spectrometry for the simultaneous determinationof baicalein, b-aicalin, oroxylin A and wogonin in rat plasma. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2006, 844, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Tong, L.; Wan, M.; Zhang, L.; Zhu, Y.; Sun, H.; Bi, K. Simultaneous determination of baicalin, w-ogonoside, baicalein, wogonin, oroxylin A and chrysin of Radixscutellariae extract in rat pla-sma by liquid chromatography tandem mass spectrometry. J. Pharm. Biomed. Anal. 2012, 70, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Zhang, L.; Cheng, L.; Mao, W. High-throughput salting-out assisted liquid-liquid extraction with acetonitrile for the determination of anandamide in plasma of hemodialysis patients with liquid chromatography tandem mass spectrometry. Biomed. Chromatogr. 2015, 29, 1317–1324. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Zhao, L. Passive lung targeted drug delivery systems via intravenous administration. Pharm. Dev. Technol. 2014, 19, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Waser, P.G.; Muller, U.; Kreuter, J.; Berger, S.; Munz, K.; Kaiser, E.; Pfluger, B. Localization of colloidal particles (liposomes, hexylcyanoacrylate nanoparticles and albumin nanoparticles) by histology and autoradigraphy in mice. Int. J. Pharm. 1987, 39, 213–227. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the baicalin loaded liposomes are available from the authors.






| Biosample | Standard Curves | Linear Ranges (μg/g or μg/mL) b | Correlation Coefficient (r) |
|---|---|---|---|
| Heart | A = 0.0967C + 0.0072 | 0.05–10 | r = 0.9997 |
| Kidney | A = 0.0866C + 0.0083 | 0.2–10 | r = 0.9996 |
| Brain | A = 0.0788C + 0.0071 | 0.05–10 | r = 0.9997 |
| Stomach | A = 0.0732C + 0.0304 | 0.05–5 | r = 0.9994 |
| Plasma | A = 0.1017C − 0.0037 | 0.05–10 | r = 0.9995 |
| Liver | A = 0.0657C + 0.0003 | 0.2–5 | r = 0.9991 |
| Spleen | A = 0.0584C + 0.0123 | 0.05–10 | r = 0.9996 |
| Lung | A = 0.059C + 0.2118 | 0.75–300 | r = 0.9992 |
| Samples | Added Concentration b | Intra-Day | Inter-Day | ||||
|---|---|---|---|---|---|---|---|
| Measured Concentration b | Accuracy (%) | (RSD) (%) | Measured Concentration b | Accuracy (%) | (RSD) (%) | ||
| Plasma | 0.0525 | 0.045 | 85.2 | 6.91 | 0.048 | 90.9 | 6.24 |
| 4.7500 | 4.223 | 88.3 | 9.06 | 4.518 | 95.2 | 8.37 | |
| 9.5000 | 7.747 | 81.6 | 8.69 | 8.527 | 89.5 | 9.64 | |
| Heart | 0.0525 | 0.044 | 83.8 | 4.42 | 0.046 | 87.4 | 4.37 |
| 4.7500 | 4.015 | 84.5 | 9.65 | 4.346 | 91.5 | 9.94 | |
| 9.5000 | 8.912 | 93.8 | 6.75 | 7.681 | 80.6 | 7.47 | |
| Liver | 0.210 | 0.191 | 91.3 | 6.52 | 0.183 | 87.2 | 6.97 |
| 2.375 | 1.926 | 81.1 | 10.24 | 2.094 | 88.4 | 10.81 | |
| 4.750 | 3.837 | 80.7 | 9.57 | 4.025 | 84.7 | 9.18 | |
| Spleen | 0.0525 | 0.047 | 88.5 | 7.97 | 0.048 | 90.4 | 7.24 |
| 4.7500 | 4.126 | 86.6 | 5.46 | 4.388 | 92.7 | 5.02 | |
| 9.5000 | 8.005 | 84.2 | 9.11 | 7.732 | 81.3 | 9.48 | |
| Lung | 0.8 | 0.663 | 82.9 | 4.19 | 0.649 | 80.8 | 4.74 |
| 142.5 | 132.245 | 92.5 | 5.64 | 119.272 | 83.7 | 5.38 | |
| 285.0 | 232.275 | 81.4 | 8.84 | 251.655 | 88.6 | 9.17 | |
| Kidney | 0.21 | 0.206 | 98.4 | 9.67 | 0.174 | 81.8 | 10.83 |
| 4.75 | 4.273 | 89.9 | 5.14 | 3.993 | 84.3 | 5.73 | |
| 9.50 | 8.829 | 92.2 | 8.42 | 8.278 | 87.6 | 8.62 | |
| Stomach | 0.0525 | 0.051 | 98.1 | 9.73 | 0.049 | 93.5 | 9.28 |
| 2.3750 | 2.137 | 90.2 | 8.03 | 1.978 | 83.3 | 8.75 | |
| 4.7500 | 4.355 | 91.3 | 10.84 | 4.235 | 89.2 | 10.73 | |
| Brain | 0.0525 | 0.049 | 95.1 | 10.64 | 0.044 | 80.9 | 10.93 |
| 4.7500 | 3.959 | 83.4 | 7.99 | 4.088 | 86.4 | 7.63 | |
| 9.500 | 8.544 | 89.3 | 8.53 | 7.947 | 83.6 | 8.28 | |
| Samples | Added Concentration (μg/mL or μg/g) b | Extraction Recovery (μg/mL or μg/g) b | RSD (%) |
|---|---|---|---|
| Plasma | 0.0525 | 85.7 | 2.51 |
| 4.75 | 88.3 | 9.28 | |
| 9.5 | 81.5 | 8.87 | |
| Heart | 0.0525 | 87.9 | 1.08 |
| 4.75 | 82.7 | 1.58 | |
| 9.5 | 86.9 | 7.14 | |
| Kidney | 0.21 | 78.7 | 9.73 |
| 4.75 | 93.2 | 9.51 | |
| 9.5 | 80.3 | 5.84 | |
| Brain | 0.0525 | 81.7 | 3.38 |
| 4.75 | 86.4 | 2.12 | |
| 9.5 | 79.2 | 3.03 | |
| Stomach | 0.0525 | 87.2 | 9.89 |
| 2.375 | 81.8 | 2.75 | |
| 4.75 | 94.6 | 6.68 | |
| Liver | 0.21 | 92.3 | 8.16 |
| 2.375 | 80.7 | 5.47 | |
| 4.75 | 73.1 | 8.58 | |
| Spleen | 0.0525 | 91.9 | 9.35 |
| 4.75 | 78.3 | 8.07 | |
| 9.5 | 81.5 | 3.21 | |
| Lung | 0.8 | 93.2 | 1.68 |
| 142.5 | 9.9 | 3.85 | |
| 285.0 | 87.1 | 8.65 |
| Freeze-Thaw Stability | Storage Stability | Post-Preparative Stability | |||||
|---|---|---|---|---|---|---|---|
| Samples | Added Concentration (μg/mL or μg/g) b | Measured Concentration (μg/mL or μg/g) b | Relative Error (%) | Measured Concentration (μg/mL or μg/g) b | Relative Error (%) | Measured Concentration (μg/mL or μg/g) b | Relative Error (%) |
| 0.0525 | 0.047 | −10.5 | 0.049 | −6.7 | 0.045 | −14.3 | |
| Plasma | 4.75 | 4.138 | −12.9 | 4.258 | −10.4 | 4.371 | −8.0 |
| 9.5 | 8.362 | −12.0 | 8.139 | −14.3 | 8.697 | −8.5 | |
| 0.0525 | 0.048 | −8.6 | 0.045 | −14.3 | 0.047 | −10.5 | |
| Heart | 4.75 | 4.154 | −12.5 | 4.123 | 13.2 | 4.472 | −5.9 |
| 9.5 | 8.118 | −14.5 | 8.767 | −7.7 | 8.93 | −6.0 | |
| 0.21 | 0.18 | −14.3 | 0.18 | −14.3 | 0.19 | −9.5 | |
| Kidney | 4.75 | 4.164 | −12.3 | 4.109 | −13.5 | 4.497 | −5.3 |
| 9.5 | 8.569 | −9.8 | 8.895 | −6.4 | 9.154 | −3.6 | |
| 0.0525 | 0.046 | −12.4 | 0.048 | −8.6 | 0.049 | −6.7 | |
| Brain | 4.75 | 4.272 | −10.1 | 4.172 | −12.2 | 4.625 | −2.6 |
| 9.5 | 8.763 | −7.8 | 8.863 | −6.7 | 9.29 | −2.2 | |
| 0.0525 | 0.045 | −14.3 | 0.048 | −8.6 | 0.047 | −10.5 | |
| Stomach | 2.375 | 2.149 | −9.5 | 2.218 | −6.6 | 2.195 | −7.6 |
| 4.75 | 4.056 | −14.6 | 4.476 | −5.8 | 4.556 | −4.1 | |
| 0.21 | 0.193 | −8.1 | 0.182 | −13.3 | 0.22 | 4.8 | |
| Liver | 2.375 | 2.068 | −12.9 | 2.122 | −10.7 | 2.389 | 0.6 |
| 4.75 | 4.054 | −14.7 | 4.365 | −8.1 | 4.891 | 3.0 | |
| 0.0525 | 0.046 | −12.4 | 0.047 | −10.5 | 0.053 | 1.0 | |
| Spleen | 4.75 | 3.956 | −16.7 | 4.556 | −4.1 | 4.689 | −1.3 |
| 9.5 | 8.252 | −13.1 | 8.589 | −9.6 | 9.138 | -3.8 | |
| 0.8 | 0.744 | −7.0 | 0.72 | −10.0 | 0.84 | 5.0 | |
| Lung | 142.5 | 125.828 | −11.7 | 130.28 | −8.6 | 135.66 | −4.8 |
| 285 | 256.35 | −10.1 | 265.79 | −6.7 | 271.45 | −4.8 | |
| Samples | t1/2α (h) | t1/2β | Cmax (μg/mL) | AUC(0–24h) (mg/L·h) | CLz (L/h/kg) | Vz (L/kg) |
|---|---|---|---|---|---|---|
| Baicalin liposomes | 0.038 | 1.02 | 0.535 * | 2.42 * | 3.51 | 51.77 |
| Baicalin injection | 0.141 | 3.88 | 1.736 | 7.07 | 1.34 | 10.27 |
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wei, Y.; Pi, C.; Yang, G.; Xiong, X.; Lan, Y.; Yang, H.; Zhou, Y.; Ye, Y.; Zou, Y.; Zheng, W.; et al. LC-UV Determination of Baicalin in Rabbit Plasma and Tissues for Application in Pharmacokinetics and Tissue Distribution Studies of Baicalin after Intravenous Administration of Liposomal and Injectable Formulations. Molecules 2016, 21, 444. https://doi.org/10.3390/molecules21040444
Wei Y, Pi C, Yang G, Xiong X, Lan Y, Yang H, Zhou Y, Ye Y, Zou Y, Zheng W, et al. LC-UV Determination of Baicalin in Rabbit Plasma and Tissues for Application in Pharmacokinetics and Tissue Distribution Studies of Baicalin after Intravenous Administration of Liposomal and Injectable Formulations. Molecules. 2016; 21(4):444. https://doi.org/10.3390/molecules21040444
Chicago/Turabian StyleWei, Yumeng, Chao Pi, Gang Yang, Xiaoming Xiong, Yongshu Lan, Hongru Yang, Yang Zhou, Yun Ye, Yonggen Zou, Wenwu Zheng, and et al. 2016. "LC-UV Determination of Baicalin in Rabbit Plasma and Tissues for Application in Pharmacokinetics and Tissue Distribution Studies of Baicalin after Intravenous Administration of Liposomal and Injectable Formulations" Molecules 21, no. 4: 444. https://doi.org/10.3390/molecules21040444





