Pharmacokinetic-Pharmacodynamic Modeling to Study the Antipyretic Effect of Qingkailing Injection on Pyrexia Model Rats
Abstract
:1. Introduction
2. Results
2.1. Pharmacokinetic Profiles of Six Analytes in Normal Treated Group and Pyrexia Model Group Rats
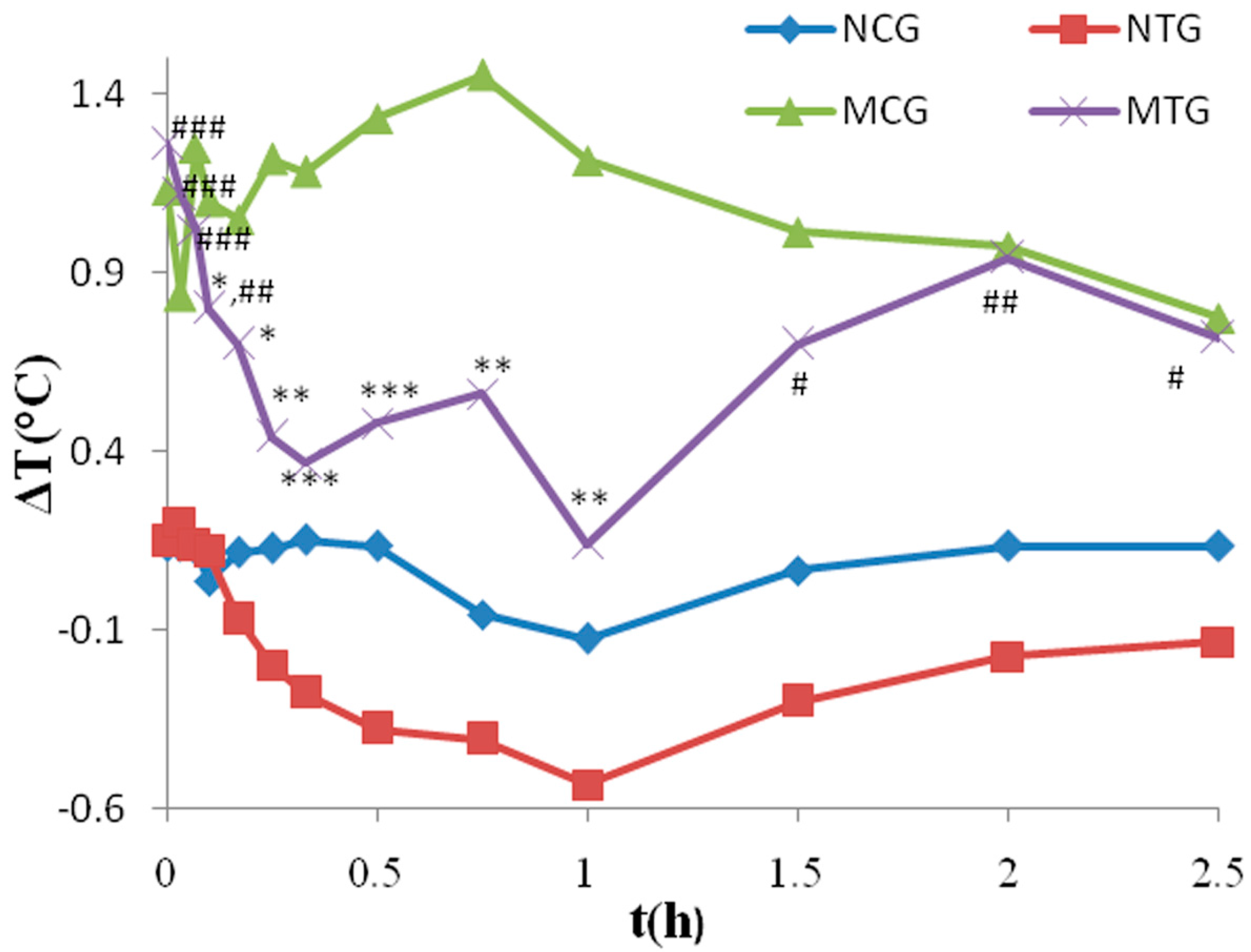
2.2. Temperature Analysis
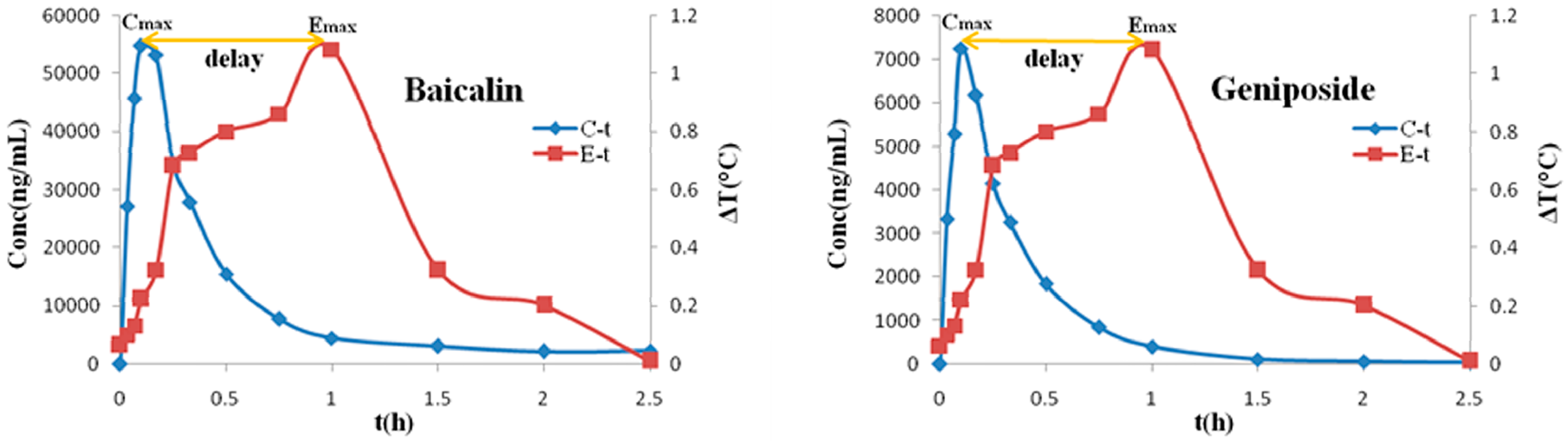
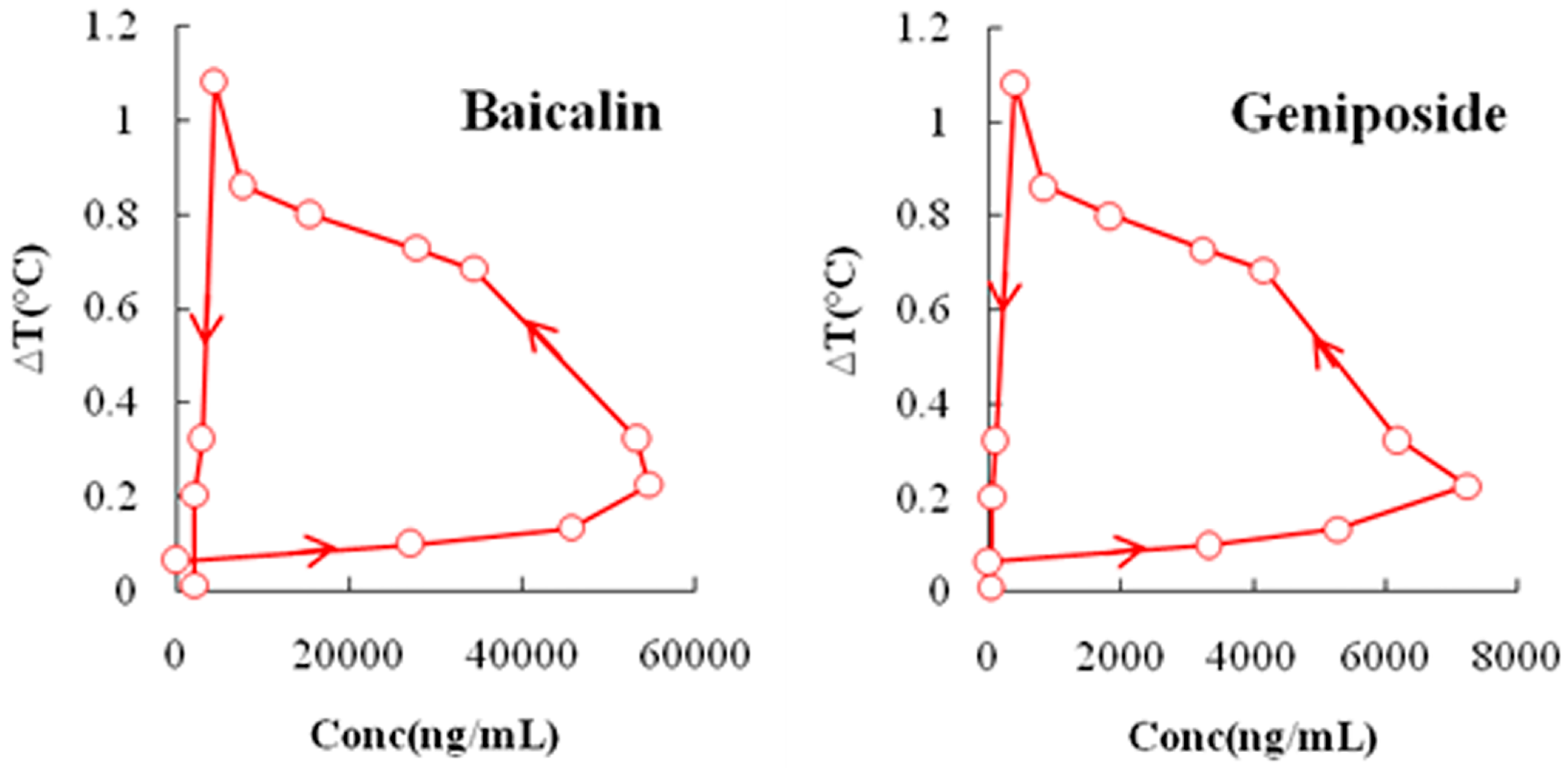
2.3. PK-PD Modeling
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Experimental Animals and Sample Collection
4.3. Analytical Determination of Plasma Samples
4.4. Pharmacokinetic Analysis
4.5. PK-PD Simulation
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Yan, S.K.; Xin, W.F.; Wang, Y.M.; Cheng, Y.Y. An approach to develop two-dimensional fingerprint for the quality control of Qingkailing injection by high-performance liquid chromatography with diode array detection. J. Chromatogr. A. 2005, 1090, 90–97. [Google Scholar] [CrossRef] [PubMed]
- The State Pharmacopoeia Commission of the P.R. China. Pharmacopoeia of the P.R. China; Chemical Industry Press: Beijing, China, 2010; pp. 1110–1111. [Google Scholar]
- Gao, X.Y. Study on the methods of online process monitoring and quality control of Qingkailing injection. Master’s Thesis, Beijing University of Chinese Medicine, Beijing, 2006. [Google Scholar]
- Gao, X.Y.; Li, N.; Fan, Q.; Wang, Y.; Qiao, Y.J. Study on the method of rapid quality control of aqueous solution of flos Ionicerae japonicae extraction in the preparation of Qingkailing injection. Spectrosc. Spect. Anal. 2006, 26, 904–907. [Google Scholar]
- Gao, X.Y.; Fan, Q.; Li, N.; Shi, X.Y.; Qiao, Y.J. Characterization and determination of nitrogen in preparation of Qingkailing injection and its intermediate products. China J. Tradit. Chin. Med. Pharm. 2008, 33, 1673–1676. [Google Scholar]
- Gao, X.Y.; Guo, M.X.; Peng, L.; Zhao, B.S.; Su, J.K.; Liu, H.Y.; Zhang, L.; Bai, X.; Qiao, Y.J. UPLC Q-TOF/MS-based metabolic profiling of urine reveals the novel antipyretic mechanisms of Qingkailing injection in a rat model of yeast-induced pyrexia. Evid. Based Complement. Altern. Med. 2013. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.X.; Zhang, L.; Liu, H.Y.; Qin, L.L.; Zhang, Z.X.; Bai, X.; Gao, X.Y. A metabolomic strategy to screen the prototype components and metabolites of Qingkailing injection in rat urine by high-performance liquid chromatography with tendem mass spectrometry. J. Sep. Sci. 2014, 37, 2844–2850. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Gao, X.Y.; Song, Y.L.; Zhao, L.S.; Guo, M.X.; Su, J.K.; Zhang, L.; Liu, H.Y. A rapid and sensitive UPLC-MS/MS method for quantification of two caffeoylquinic acids and four main active components in rat plasma after an intravenous administration of Qingkailing injection and its application to a pharmacokinetic study. Biomed. Chromatogr. 2013, 28, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, X.; Su, J.K.; Liu, H.Y.; Zhang, Z.X.; Qin, L.L.; He, C.; Peng, L.; Guo, M.X.; Gao, X.Y. One single amino acid for estimation the content of total free amino acids in Qingkailing injection using high-performance liquid chromatography-diode array detection. J. Anal. Methods Chem. 2014. [Google Scholar] [CrossRef] [PubMed]
- Ji, K.M.; Chen, J.J.; Li, M.; Liu, Z.G.; Xia, L.X.; Wang, C.B.; Zhan, Z.K.; Wu, X.L. Comments on serious anaphylaxis caused by nine Chinese herbal injections used to treat common colds and upper respiratory tract infections. Regul. Toxicol. Pharmacol. 2009, 55, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.L.; Lees, P. Integration and modelling of pharmacokinetic and pharmacodynamic data to optimize dosage regimens in veterinary medicine. J. Vet. Pharmacol. Ther. 2004, 27, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Aliabadi, F.S.; Landoni, M.F.; Lees, P. Pharmacokinetics (PK), pharmacodynamics (PD), and PK-PD integration of danofloxacin in sheep biological fluids. Antimicrob. Agents Chemother. 2003, 47, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yu, J.C.; Shi, Y.G.; Zhou, L.; Ye, X.Y.; Zhu, D.S.; Zhang, Y.Y. Study of pharmacokinetics/pharmacodynamics of levofloxacin. Natl. Med. J. China 2005, 85, 1926–1932. [Google Scholar]
- Haritova, A.M.; Rusenova, N.V.; Parvanov, P.R.; Lashev, L.D.; Fink-Gremmels, J. Integration of pharmacokinetic and pharmacodynamic indices of Marbofloxacin in turkeys. Antimicrob. Agents Chemother. 2006, 50, 3779–3785. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, D.; Tauber, J.; Reis, B.L. Efficacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-severe dry eye disease: A dose-ranging, randomized trial. The cyclosporine a phase 2 study group. Ophthalmology 2000, 107, 967–974. [Google Scholar] [CrossRef]
- Bray, G.A.; Hollander, P.; Klein, S.; Kushner, R.; Levy, B.; Fitchet, M.; Perry, B.H. A 6-month randomized, placebo-controlled, dose-ranging trial of topiramate for weight loss in obesity. Obes. Res. 2003, 11, 722–733. [Google Scholar] [CrossRef] [PubMed]
- Emery, P.; Fleischmann, R.; Filipowicz-Sosnowska, A.; Schechtman, J.; Szczepanski, L.; Kavanaugh, A.; Racewicz, A.J.; van Vollenhoven, R.F.; Li, N.F.; Aqarwal, S.; et al. The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: Results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum. 2006, 54, 1390–1400. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.P.; Hibbeln, J.R.; Wisner, K.L.; Brumbach, B.H.; Watchman, M.; Gelenberg, A.J. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta. Psychiatr. Scand. 2006, 113, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.L.; Cester, C.C.; Haak, T.; Laroute, V. A pharmacokinetic/pharmacodynamic approach vs. a dose titration for the determination of a dosage regimen: The case of nimesulide, a Cox-2 selective nonsteroidal anti-inflammatory drug in the dog. J. Vet. Pharmacol. Ther. 2001, 24, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Chien, Y.W. Pharmacokinetic-pharmacodynamic modelling of insulin: Comparison of indirect pharmacodynamic response with effect-compartment link models. J. Pharm. Pharmacol. 2002, 54, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Höcht, C.; Diverniero, C.; Opezzo, J.A.; Taira, C.A. Applicability of microdialysis as a technique for pharmacokinetic-pharmacodynamic (PK-PD) modeling of antihypertensive beta-blockers. J. Pharmacol. Toxicol. Methods 2005, 52, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Bertera, F.M.; Mayer, M.A.; Opezzo, J.A.; Taira, C.A.; Höcht, C. Comparison of different pharmacodynamic models for PK-PD modeling of verapamil in renovascular hypertension. J. Pharmacol. Toxi. Methods 2008, 57, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Olsen, C.K.; Brennum, L.T.; Kreilgaard, M. Using pharmacokinetic-pharmacodynamic modelling as a tool for prediction of therapeutic effective plasma levels of antipsychotics. Eur. J. Pharmacol. 2008, 584, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Bertera, F.M.; Mayer, M.A.; Opezzo, J.A.; Taira, C.A.; Höcht, C. Increased sensitivity to diltiazem hypotensive effect in an experimental model of high-renin hypertension. J. Pharm. Pharmacol. 2009, 61, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhang, X.Y.; Chen, G.K. Adverse effect and mechanism of chlorogenic acid in clearing heat and detoxication traditional Chinese medicine injections. Chin. J. Mod. Appl. Pharm. 2009, 7, 555–558. [Google Scholar]
- Li, B.Q.; Dong, X.; Yang, G.Q.; Fang, S.H.; Gao, J.Y.; Zhang, J.X.; Gu, F.M.; Miao, X.M.; Zhao, H. Role of chlorogenic acid in the toxicity induced by Chinese herbal injections. Drug Chem. Toxicol. 2010, 33, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; He, R.; Xu, Q.H.; Gao, J.; Lu, Y.L.; Li, J.R. Effect of chlorogenic acid on degranulation in mast cell RBL-2H3. China J. Chin. Mater. Med. 2011, 36, 912–916. [Google Scholar]
- Refinetti, R.; Ma, H.; Satinoff, E. Body temperature rhythms, cold tolerance, and fever in young and old rats of both genders. Exp. Gerontol. 1990, 25, 533–543. [Google Scholar] [CrossRef]
- Makonnen, E.; Debella, A.; Zerihun, L.; Abebe, D.; Teka, F. Antipyretic properties of the aqueous and ethanol extracts of the leaves of Ocimum suave and Ocimum lamiifolium in mice. J. Ethnopharmacol. 2003, 88, 85–91. [Google Scholar] [CrossRef]
- Devi, B.P.; Boominathan, R.; Mandal, S.C. Anti-inflammatory, analgesic and antipyretic properties of Clitoria ternatearoot. Fitoterapia 2003, 74, 345–349. [Google Scholar] [CrossRef]
- Bhat, A.S.; Tandan, S.K.; Kumar, D.; Krishna, V.; Prakash, V.R. Interaction between inhibitors of inducible nitric oxide synthase and cyclooxygenase in Brewer’s yeast induced pyrexia in mice: An isobolographic study. Eur. J. Pharmacol. 2005, 511, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Bafor, E.E.; Uwumarongie, H.O.; Idiake, J.O. Antipyretic effects of the aqueous, ethyl acetate and hexane leaf extracts of Ficus exasperata (Moraceae) in mice. J. Therm. Biol. 2010, 35, 275–279. [Google Scholar] [CrossRef]
- Wang, H.; Chen, J.M.; Zhang, Q.G. High-performance liquid chromatographic determination of baicalin in human plasma. J. Shenyang Pharm. Univ. 2000, 17, 107–109. [Google Scholar]
- Tang, Y.H.; Zhu, H.Y.; Zhang, Y.Y.; Huang, C.G. Determination of human plasma protein binding of baicalin by ultrafiltration and high-performance liquid chromatography. Biomed. Chromatogr. 2006, 20, 1116–1119. [Google Scholar] [CrossRef] [PubMed]
- Holford, N.H.; Sheiner, L.B. Understanding the dose-effect relationship: Clinical application of pharmacokinetic-pharmacodynamic models. Clin. Pharmacokinet. 1981, 6, 429–453. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.L. Pharmacokinetic/pharmacodynamic integration in drug development and dosage-regimen optimization for veterinary medicine. AAPS PharmSci. 2002, 4, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Sample Availability: Samples of the compounds Qingkailing injection (QKLI), yeast, baicalin, geniposide, cholic acid, hyodeoxycholic acid, chlorogenic acid and neochlorogenic acid are available from the authors.
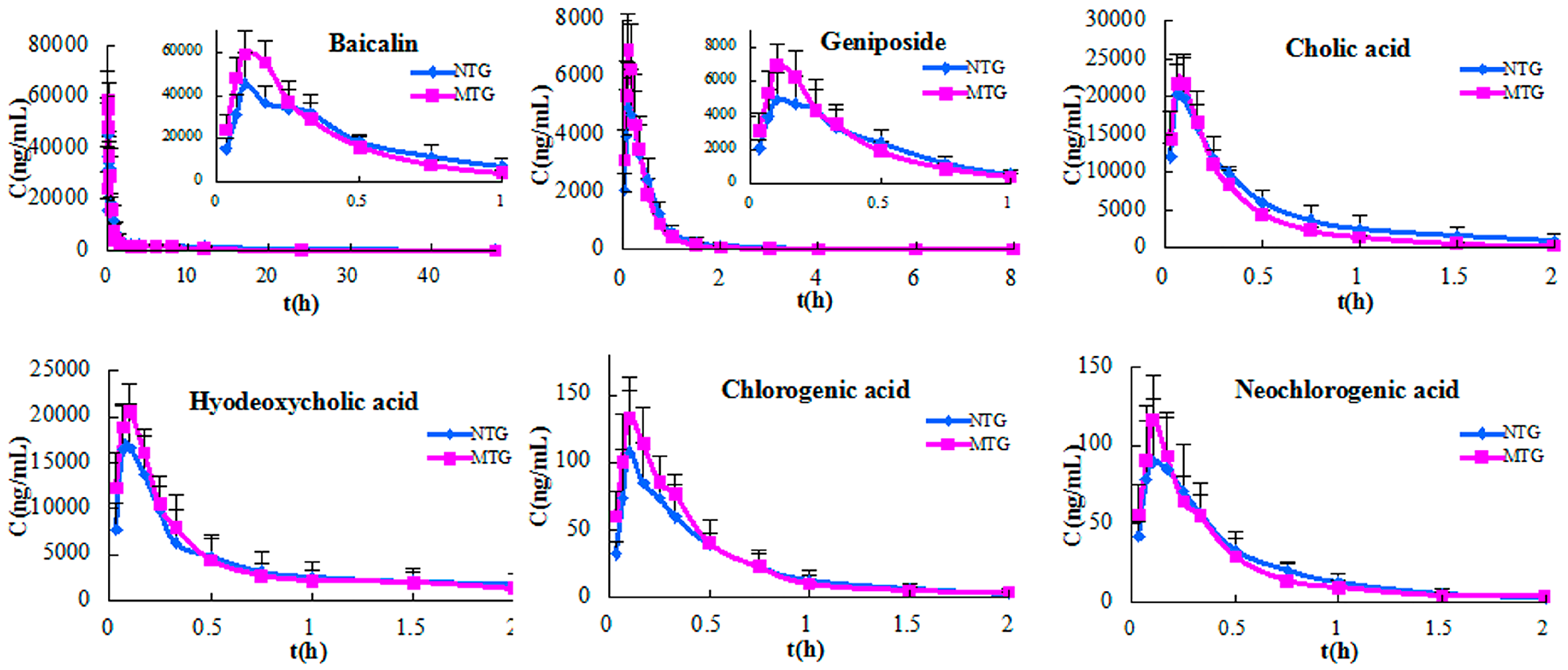
| PK Parameter | Baicalin | Geniposide | Cholic Acid | Hyodeoxycholic Acid | Chlorogenic Acid | Neochlorogenic Acid | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NTG | MTG | NTG | MTG | NTG | MTG | NTG | MTG | NTG | MTG | NTG | MTG | |
| t1/2 (h) | 12.32 ± 0.99 | 10.34 ± 0.61 | 1.90 ± 0.83 | 1.93 ± 0.43 | 0.61 ± 0.12 | 0.56 ± 0.26 | 0.64 ± 0.11 | 0.68 ± 0.04 | 0.32 ± 0.10 | 0.34 ± 0.11 | 0.24 ± 0.06 | 0.24 ± 0.05 |
| tmax (h) | 0.112 ± 0.029 | 0.142 ± 0.038 | 0.123 ± 0.036 | 0.135 ± 0.038 | 0.074 ± 0.015 | 0.093 ± 0.015 | 0.089 ± 0.017 | 0.114 ± 0.031 | 0.147 ± 0.036 | 0.134 ± 0.071 | 0.135 ± 0.038 | 0.143 ± 0.087 |
| Cmax (ng/mL) | 45,452.3 ± 14,647.02 | 59,063.86 ± 5387.80 * | 5044.57 ± 1690.17 | 7083.28 ± 738.70 * | 20,698.88 ± 5614.00 | 22,019.43 ± 3237.81 | 16,731.13 ± 4819.31 | 20,312.59 ± 2651.40 | 101.90 ± 42.26 | 125.70 ± 32.55 | 94.13 ± 40.16 | 110.58 ± 21.98 |
| AUC0-t (h·ng/mL) | 51,016.23 ± 3566.65 | 67,832.84 ± 8114.55 * | 2979.17 ± 581.50 | 2655.71 ± 536.63 | 10,038.96 ± 2720.33 | 8159.23 ± 1215.33 | 9297.71 ± 3099.90 | 9377.2 ± 2805.95 | 49.34 ± 13.19 | 53.93 ± 14.60 | 43.95 ± 12.40 | 44.54 ± 7.64 |
| AUC0-∞ (h·ng/mL) | 52,575.02 ± 3767.03 | 71,530.32 ± 8373.62 * | 2999.47 ± 582.40 | 2670.90 ± 533.86 | 10,329.32 ± 2750.36 | 8426.33 ± 1324.79 | 9585.43 ± 3101.21 | 9789.65 ± 3114.40 | 51.08 ± 12.51 | 56.44 ± 15.86 | 44.58 ± 12.45 | 45.42 ± 7.96 |
| MRT0-t (h) | 9.85 ± 0.83 | 8.22 ± 0.85 | 0.64 ± 0.17 | 0.47 ± 0.06 | 0.61 ± 0.19 | 0.48 ± 0.09 | 0.76 ± 0.18 | 0.68 ± 0.09 | 0.45 ± 0.10 | 0.40 ± 0.08 | 0.43 ± 0.09 | 0.38 ± 0.06 |
| MRT0-∞ (h) | 12.77 ± 1.00 | 9.84 ± 0.90 | 0.71 ± 0.17 | 0.53 ± 0.05 | 0.70 ± 0.22 | 0.57 ± 0.15 | 0.86 ± 0.20 | 0.80 ± 0.11 | 0.52 ± 0.14 | 0.47 ± 0.12 | 0.45 ± 0.11 | 0.41 ± 0.06 |
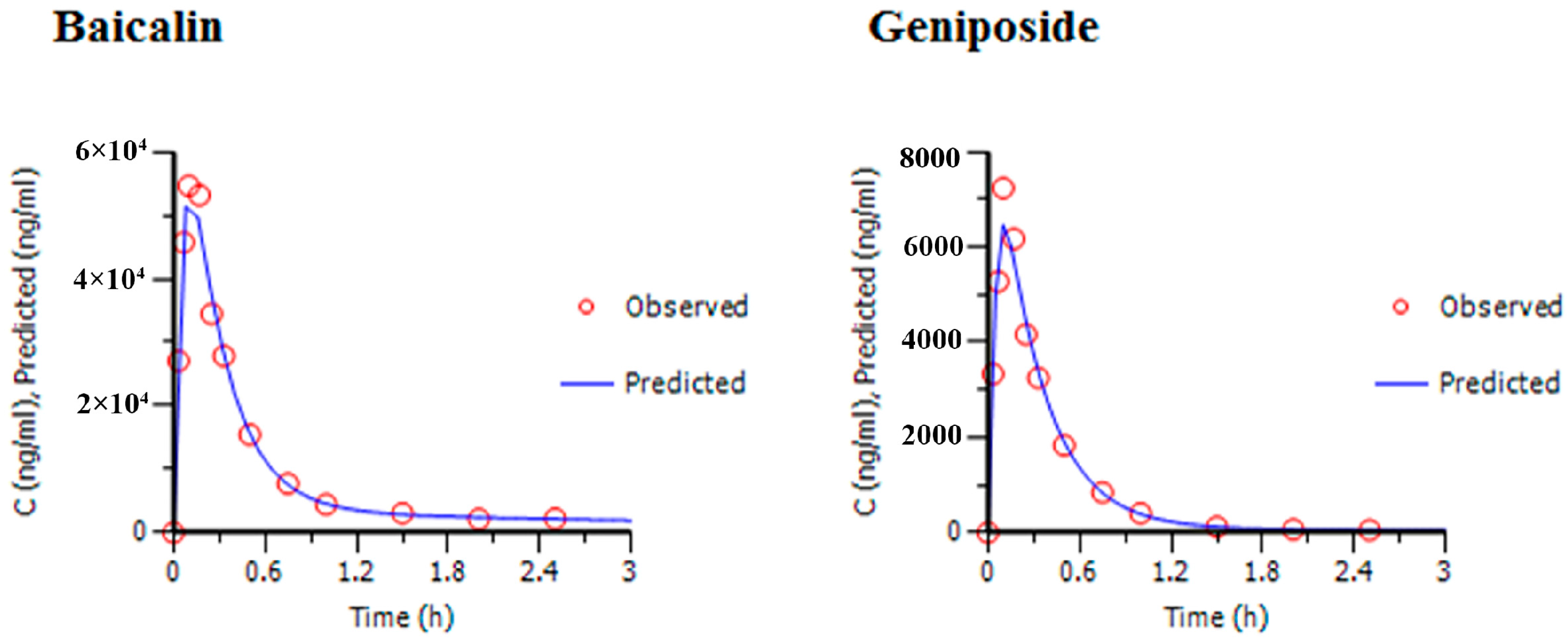
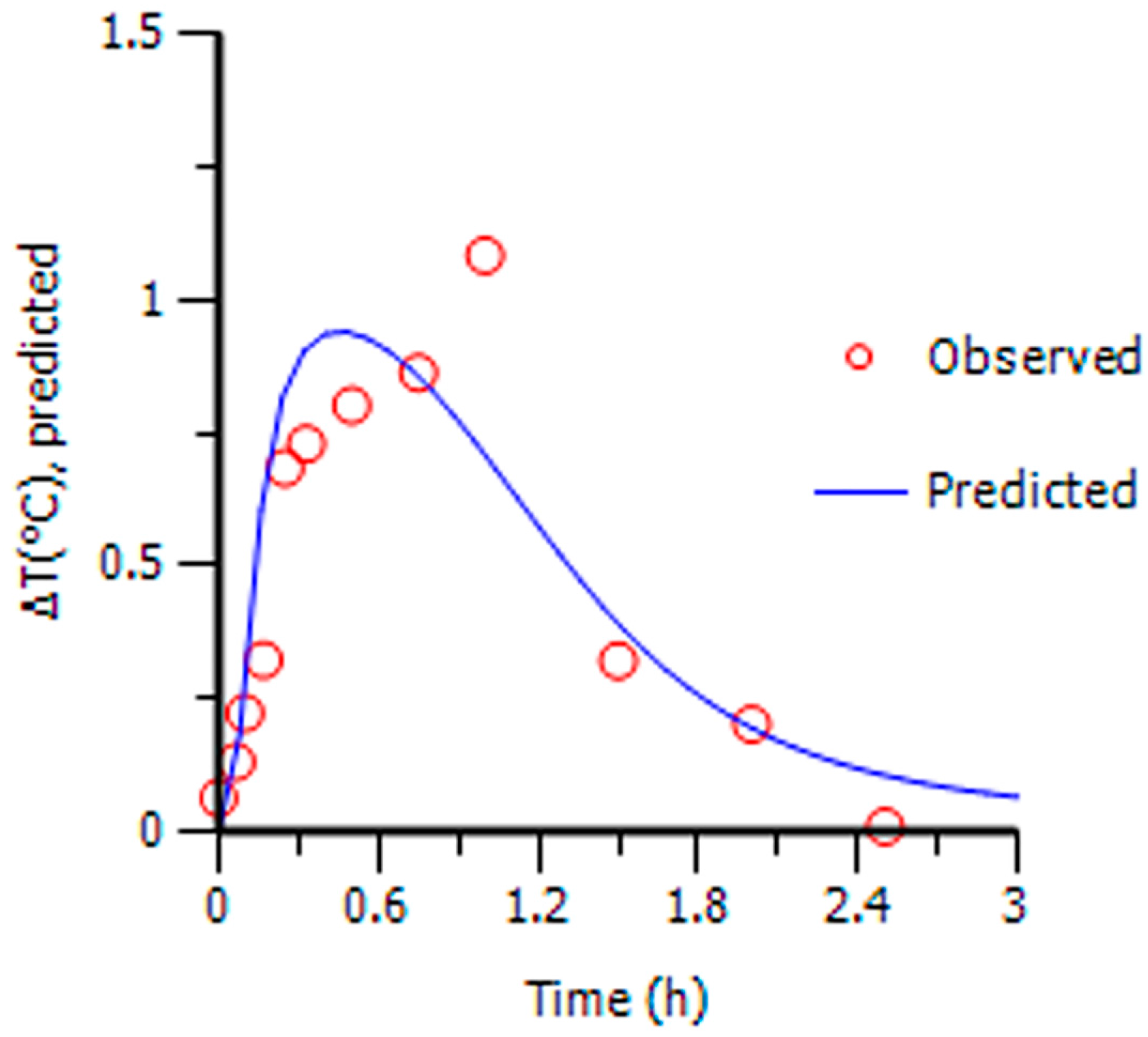
| t (h) | C (ng/mL) | ∆T (°C) | |
|---|---|---|---|
| Baicalin | Geniposide | ||
| 0 | 0 | 0 | 0.065 |
| 0.033 | 23,053 ± 1533.71 | 3777.28 ± 1060.57 | 0.098 |
| 0.067 | 46,133.46 ± 3300.19 | 5616.80 ± 668.04 | 0.132 |
| 0.1 | 54,852.34 ± 5601.30 | 6921.36 ± 659.57 | 0.224 |
| 0.17 | 56,117.21 ± 8107.36 | 6684.34 ± 741.91 | 0.324 |
| 0.25 | 32,275.86 ± 7226.69 | 4248.63 ± 1139.85 | 0.684 |
| 0.33 | 19,552.27 ± 5468.90 | 3280.44 ± 799.09 | 0.729 |
| 0.5 | 13,953.74 ± 5684.01 | 1739.75 ± 560.55 | 0.801 |
| 0.75 | 6173.46 ± 2291.78 | 762.76 ± 404.31 | 0.862 |
| 1.0 | 3587.83 ± 929.05 | 322.06 ± 207.30 | 1.082 |
| 1.5 | 2536.16 ± 310.87 | 68.59 ± 23.30 | 0.382 |
| 2.0 | 2224.68 ± 206.74 | 42.08 ± 22.52 | 0.253 |
| 2.5 | 2050.67 ± 249.00 | 36.64 ± 19.13 | 0.081 |
| Compound | Emax (°C) | EC50 (ng/mL) | γ | ke0 (1/h) |
|---|---|---|---|---|
| Baicalin | 1.31 | 10,944.43 | 2.03 | 1.59 |
| Geniposide | 1.23 | 1094.33 | 2.08 | 1.35 |
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Qin, L.; Peng, L.; Zhang, Q.; Wang, Q.; Lu, Z.; Song, Y.; Gao, X. Pharmacokinetic-Pharmacodynamic Modeling to Study the Antipyretic Effect of Qingkailing Injection on Pyrexia Model Rats. Molecules 2016, 21, 317. https://doi.org/10.3390/molecules21030317
Zhang Z, Qin L, Peng L, Zhang Q, Wang Q, Lu Z, Song Y, Gao X. Pharmacokinetic-Pharmacodynamic Modeling to Study the Antipyretic Effect of Qingkailing Injection on Pyrexia Model Rats. Molecules. 2016; 21(3):317. https://doi.org/10.3390/molecules21030317
Chicago/Turabian StyleZhang, Zhixin, Lingling Qin, Long Peng, Qingqing Zhang, Qing Wang, Zhiwei Lu, Yuelin Song, and Xiaoyan Gao. 2016. "Pharmacokinetic-Pharmacodynamic Modeling to Study the Antipyretic Effect of Qingkailing Injection on Pyrexia Model Rats" Molecules 21, no. 3: 317. https://doi.org/10.3390/molecules21030317






