Urinary Metabolomic Profiling Reveals the Effect of Shenfu Decoction on Chronic Heart Failure in Rats
Abstract
:1. Introduction
2. Results and Discussion
2.1. Hemodynamic Assessment
| Time (week) | Group | LVSP (mmHg) | LVEDP (mmHg) | +dp/dtmax (mmHg) | −dp/dtmax (mmHg) |
|---|---|---|---|---|---|
| 8 | Normal Controls | 174.70 ± 2.06 | −16.68 ± 2.42 | 7455.01 ± 643.01 | −4964.79 ± 749.17 |
| Sham Surgery | 152.54 ± 27.96 | −18.61 ± 4.85 | 5916.10 ± 779.03 | −4677.67 ± 656.71 | |
| CHF group | 120.81 ± 11.40 Δ,* | 2.09 ± 0.10 Δ,* | 2622.39 ± 744.60 Δ,* | −2357.32 ± 482.95 Δ,* | |
| 11 | Normal Controls | 137.33 ± 13.27 | −5.38 ± 3.01 | 12019.08 ± 732.35 | −9542.12 ± 1101.26 |
| Sham Surgery | 128.20 ± 6.98 | −7.73 ± 3.43 | 9312.59 ± 1312.69 | −8106.91 ± 634.04 | |
| CHF group | 105.46 ± 4.37 Δ,* | 2.84 ± 0.74 Δ,* | 6694.55 ± 712.63 Δ,* | −6925.12 ± 483.54 Δ,* | |
| SFD-treated | 125.28 ± 6.25 # | −2.60 ± 1.64 # | 8453.47 ± 979.84 # | −8565.22 ± 942.11 # |
2.2. Urinary Metabolite Profiling in Rats by GC–MS
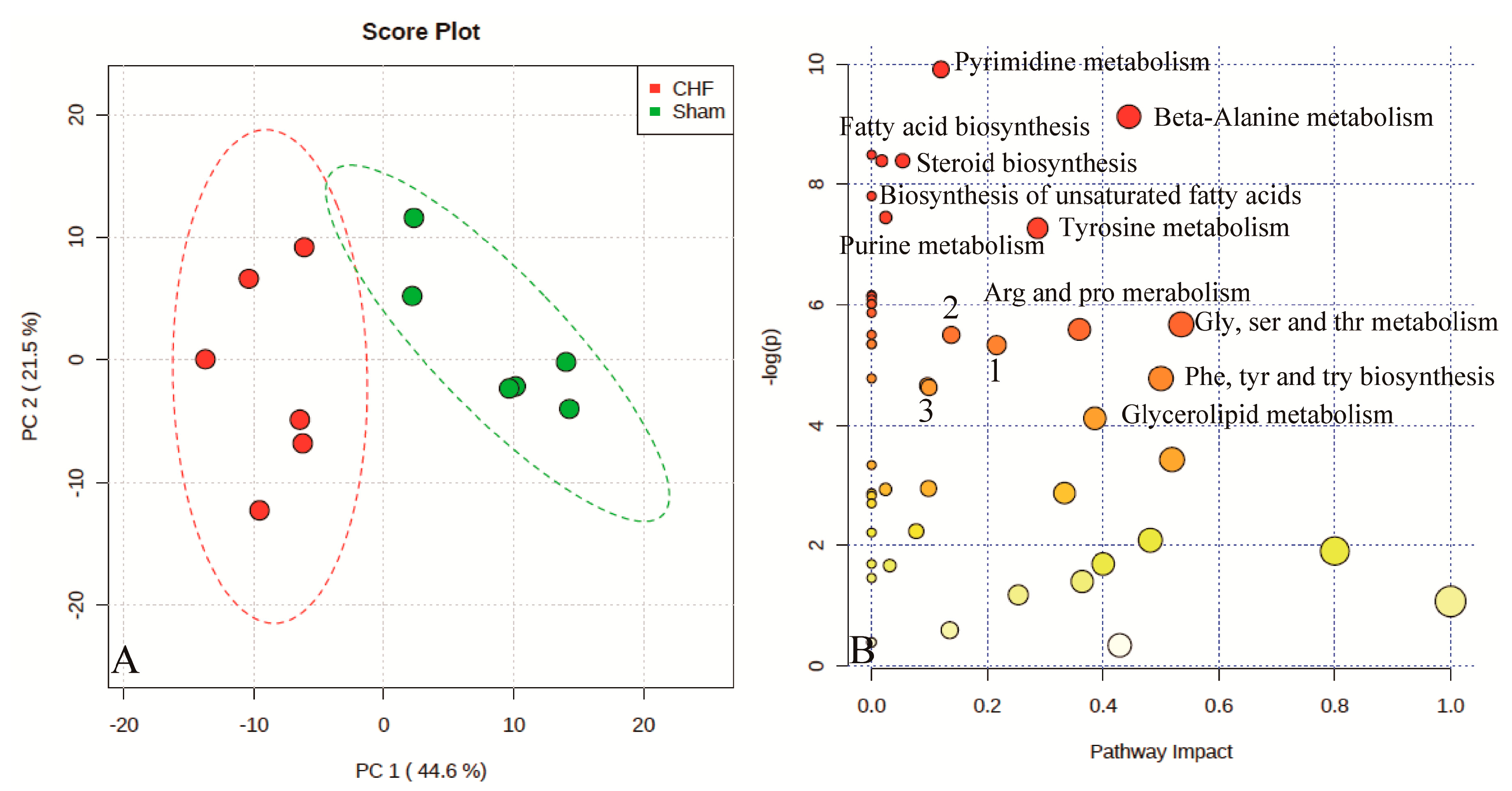
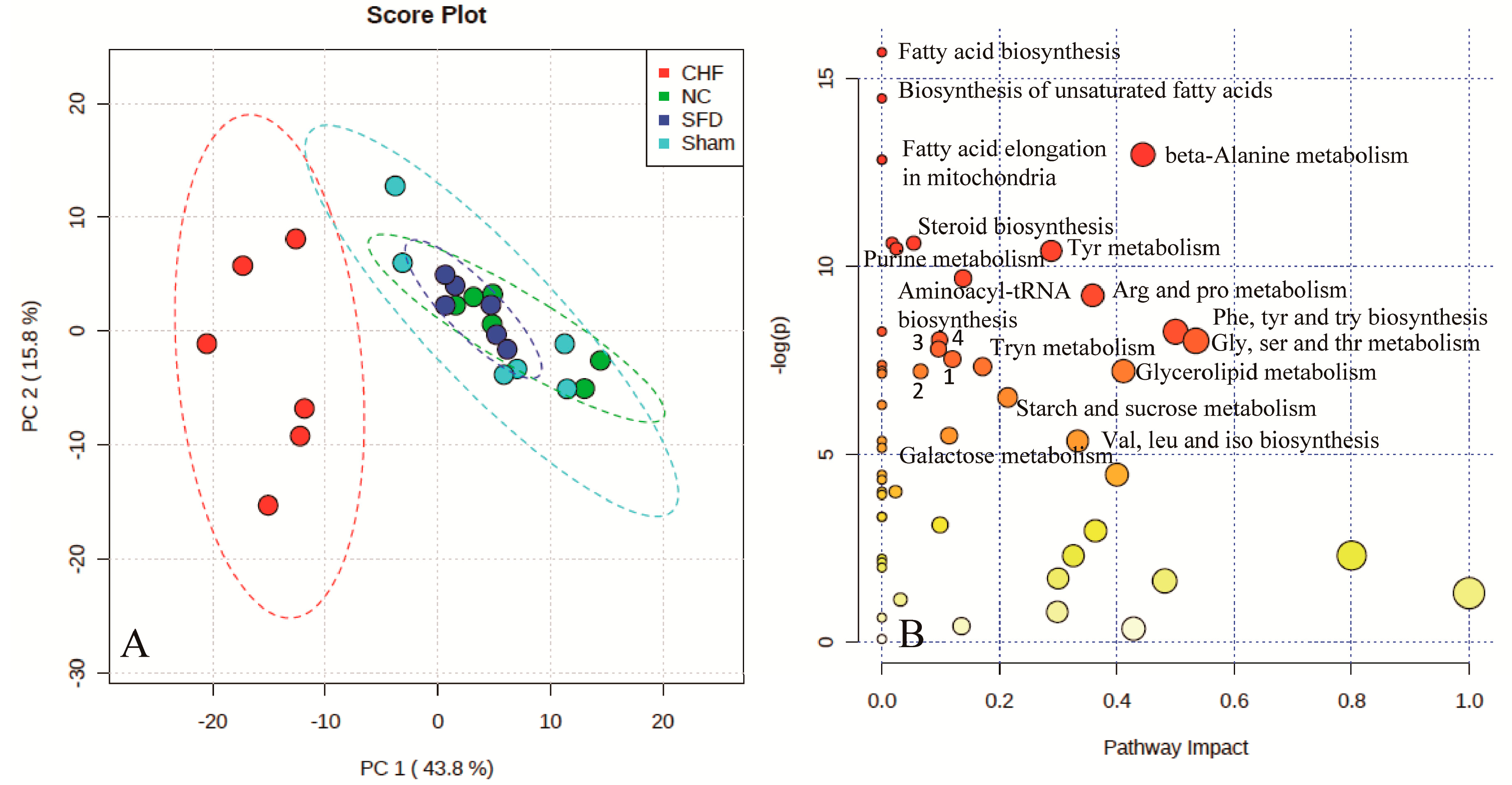
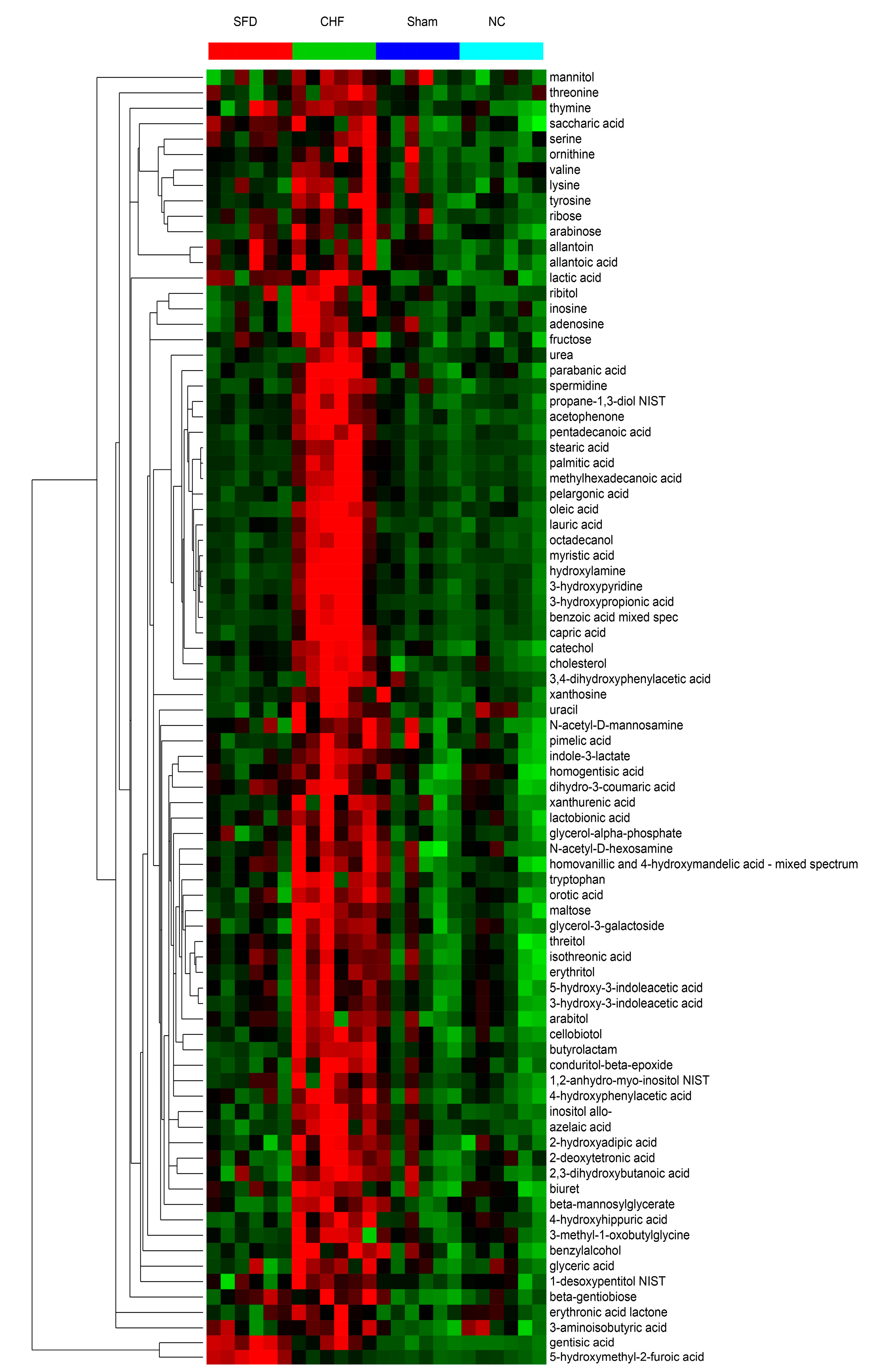
2.3. Evaluation of SFD Therapeutic Efficacy
2.4. Discussion

3. Experimental Section
3.1. Ethics Statement
3.2. Chemical Reagents and Materials
3.3. Animal Models
3.4. Extraction of Metabolites from Urine
3.5. GC–TOF–MS Analysis of Urine Extract
3.6. GC–TOF–MS Data Analysis
3.7. Statistical Analysis
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dickstein, K.; Cohen‐Solal, A.; Filippatos, G.; McMurray, J.J.; Ponikowski, P.; Poole-Wilson, P.A.; Strömberg, A.; Veldhuisen, D.J.; Atar, D.; Hoes, A.W. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur. J. Heart Fail. 2008, 10, 933–989. [Google Scholar] [CrossRef] [PubMed]
- Hunt, S.A.; Abraham, W.T.; Chin, M.H.; Feldman, A.M.; Francis, G.S.; Ganiats, T.G.; Jessup, M.; Konstam, M.A.; Mancini, D.M.; Michl, K. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2005, 112, e154–e235. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Huang, G.; He, J. Investigation of prevalence and distributing feature of chronic heart failure in Chinese adult population. Zhonghua Xin Xue Guan Bing Za Zhi 2002, 31, 3–6. [Google Scholar]
- McMurray, J.; Stewart, S. The burden of heart failure. Eur. Heart J. Suppl 2002, 4 (Suppl D), D50–D58. [Google Scholar] [CrossRef]
- Costanzo, M.R.; Guglin, M.E.; Saltzberg, M.T.; Jessup, M.L.; Bart, B.A.; Teerlink, J.R.; Jaski, B.E.; Fang, J.C.; Feller, E.D.; Haas, G.J. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J. Am. Coll. Cardiol. 2007, 49, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Sleight, P.; Pogue, J.; Bosch, J.; Davies, R.; Dagenais, G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N. Engl. J. Med. 2000, 342, 145–153. [Google Scholar] [PubMed]
- López-Sendó, J.; Swedberg, K.; McMurray, J.; Tamargo, J.; Maggioni, A.P.; Dargie, H.; Tendera, M.; Waagstein, F.; Kjekshus, J.; Lechat, P. Expert consensus document on β-adrenergic receptor blockers The Task Force on Beta-Blockers of the European Society of Cardiology. Eur. Heart J. 2004, 25, 1341–1362. [Google Scholar]
- Torabi, A.; Cleland, J.G.; Khan, N.K.; Loh, P.H.; Clark, A.L.; Alamgir, F.; Caplin, J.L.; Rigby, A.S.; Goode, K. The timing of development and subsequent clinical course of heart failure after a myocardial infarction. Eur. Heart J. 2008, 29, 859–870. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Yao, Y.; Chen, H.; Kwong, J.; Chen, J. Shengmai (a traditional Chinese herbal medicine) for heart failure. Cochrane Database Syst. Rev. 2012, 11. [Google Scholar] [CrossRef]
- Tan, G.; Liao, W.; Dong, X.; Yang, G.; Zhu, Z.; Li, W.; Chai, Y.; Lou, Z. Metabonomic profiles delineate the effect of traditional Chinese medicine Sini decoction on myocardial infarction in rats. PLoS ONE 2012, 7, e34157. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Chen, X.; Liang, Q.; Zhang, H.; Hu, P.; Wang, Y.; Luo, G. Metabonomic study of Chinese medicine Shuanglong formula as an effective treatment for myocardial infarction in rats. J. Proteome Res 2010, 10, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.; Zhang, J.; Menniti-Ippolito, F.; Gao, X.; Galeotti, F.; Massari, M.; Hu, L.; Zhang, B.; Ferrelli, R.; Fauci, A. Huangqi injection (a traditional Chinese patent medicine) for chronic heart failure: A systematic review. PLoS ONE 2011, 6, e19604. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Min, S.; Wei, K.; Cao, J. Ion channel mechanism and ingredient bases of Shenfu Decoction’s cardiac electrophysiological effects. J. Ethnopharmacol. 2008, 117, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, R.; Vaidyanathan, S.; Dunn, W.B.; Harrigan, G.G.; Kell, D.B. Metabolomics by numbers: Acquiring and understanding global metabolite data. Trends Biotechnol. 2004, 22, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Lamers, R.J.A.; Korthout, H.A.; van Nesselrooij, J.H.; Witkamp, R.F.; van der Heijden, R.; Voshol, P.J.; Havekes, L.M.; Verpoorte, R.; van der Greef, J. Metabolomics in the context of systems biology: Bridging traditional Chinese medicine and molecular pharmacology. Phytother. Res. 2005, 19, 173–182. [Google Scholar] [CrossRef]
- Wang, X.; Sun, H.; Zhang, A.; Sun, W.; Wang, P.; Wang, Z. Potential role of metabolomics apporoaches in the area of traditional Chinese medicine: As pillars of the bridge between Chinese and Western medicine. J. Pharmaceut. Biomed. 2011, 55, 859–868. [Google Scholar] [CrossRef] [PubMed]
- Dettmer, K.; Aronov, P.A.; Hammock, B.D. Mass spectrometry—Based metabolomics. Mass Spectrom. Rev. 2007, 26, 51–78. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Wu, H.; Tjeerdema, R.S.; Viant, M.R. Evaluation of metabolite extraction strategies from tissue samples using NMR metabolomics. Metabolomics 2007, 3, 55–67. [Google Scholar] [CrossRef]
- Yang, D.; Zhang, Y.; Barupal, D.K.; Fan, X.; Gustafson, R.; Guo, R.; Fiehn, O. Metabolomics of photobiological hydrogen production induced by CCCP in Chlamydomonas reinhardtii. Int. J. Hydrogen. Energ. 2014, 39, 150–158. [Google Scholar] [CrossRef]
- Kim, S.; Lee, D.Y.; Wohlgemuth, G.; Park, H.S.; Fiehn, O.; Kim, K.H. Evaluation and optimization of metabolome sample preparation methods for Saccharomyces cerevisiae. Anal. Chem. 2013, 85, 2169–2176. [Google Scholar] [CrossRef] [PubMed]
- Budczies, J.; Brockmöller, S.F.; Müller, B.M.; Barupal, D.K.; Richter-Ehrenstein, C.; Kleine-Tebbe, A.; Griffin, J.L.; Orešič, M.; Dietel, M.; Denkert, C. Comparative metabolomics of estrogen receptor positive and estrogen receptor negative breast cancer: Alterations in glutamine and beta-alanine metabolism. J. Proteomics 2013, 94, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Kind, T.; Wohlgemuth, G.; Lee, D.Y.; Lu, Y.; Palazoglu, M.; Shahbaz, S.; Fiehn, O. FiehnLib: Mass spectral and retention index libraries for metabolomics based on quadrupole and time-of-flight gas chromatography/mass spectrometry. Anal. Chem. 2009, 81, 10038–10048. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.H.; Kraus, W.E.; Newgard, C.B. Metabolomic Profiling for the Identification of Novel Biomarkers and Mechanisms Related to Common Cardiovascular Diseases Form and Function. Circulation 2012, 126, 1110–1120. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhou, M.; Sun, H.; Wang, Y. Branched-chain amino acid metabolism in heart disease: An epiphenomenon or a real culprit? Cardiovasc. Res. 2011, 90, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Desmoulin, F.; Galinier, M.; Trouillet, C.; Berry, M.; Delmas, C.; Turkieh, A.; Massabuau, P.; Taegtmeyer, H.; Smih, F.; Rouet, P. Metabonomics analysis of plasma reveals the lactate to cholesterol ratio as an independent prognostic factor of short-term mortality in acute heart failure. PLoS ONE 2013, 8, e60737. [Google Scholar] [CrossRef] [PubMed]
- Weatherill, A.R.; Lee, J.Y.; Zhao, L.; Lemay, D.G.; Youn, H.S.; Hwang, D.H. Saturated and polyunsaturated fatty acids reciprocally modulate dendritic cell functions mediated through TLR4. J. Immunol. 2005, 174, 5390–5397. [Google Scholar] [CrossRef] [PubMed]
- Staiger, H.; Staiger, K.; Stefan, N.; Wahl, H.G.; Machicao, F.; Kellerer, M.; Häring, H.U. Palmitate-induced interleukin-6 expression in human coronary artery endothelial cells. Diabetes 2004, 53, 3209–3216. [Google Scholar] [CrossRef] [PubMed]
- Eltzschig, H.K.; Bonney, S.K.; Eckle, T. Attenuating myocardial ischemia by targeting A2B adenosine receptors. Trends Mol. Med. 2013, 19, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Layland, J.; Carrick, D.; Lee, M.; Oldroyd, K.; Berry, C. Adenosine: Physiology, Pharmacology, and Clinical Applications. JACC Cardiovasc. Interv. 2014, 7, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Quintana, M.; Kahan, T.; Hjemdahl, P. Pharmacological prevention of reperfusion injury in acute myocardial infarction. Am. J. Cardiovasc. Drugs 2004, 4, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Boesten, D.M.; Berger, A.; de Cock, P.; Dong, H.; Hammock, B.D.; den Hartog, G.J.; Bast, A. Multi-targeted mechanisms underlying the endothelial protective effects of the diabetic-safe sweetener erythritol. PLoS ONE 2013, 8, e65741. [Google Scholar] [CrossRef] [PubMed]
- Hui, H.; Tang, G.; Go, V.L. Hypoglycemic herbs and their action mechanisms. Chin. Med. 2009, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, P.S.; Minicucci, M.F.; Santos, P.P.; Paiva, S.A.; Zornoff, L.A. Energy metabolism in cardiac remodeling and heart failure. Cardiol. Rev. 2013, 21, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Liu, M.; Yang, D.; Huang, Y.; Niu, X.; Wu, R.; Liu, Y.; Ma, G.; Dou, D. Quantitative LC–MS/MS analysis of seven ginsenosides and three aconitum alkaloids in Shen-Fu decoction. Chem. Cent. J. 2013, 7, 165. [Google Scholar] [CrossRef] [PubMed]
- Gaballa, M.A.; Goldman, S. Ventricular remodeling in heart failure. J. Card. Fail. 2002, 8, S476–S485. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, X.; Ren, B.; Rupp, H.; Takeda, N.; Dhalla, N.S. Modification of myosin gene expression by imidapril in failing heart due to myocardial infarction. J. Mol. Cell. Cardiol. 2002, 34, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Hearse, D.J.; Sutherland, F.J. Experimental models for the study of cardiovascular function and disease. Pharmacol. Res. 2000, 41, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Song, I.S.; Lee, D.Y.; Shin, M.H.; Kim, H.; Ahn, Y.G.; Park, I.; Kim, K.H.; Kind, T.; Shin, J.G.; Fiehn, O. Pharmacogenetics meets metabolomics: Discovery of tryptophan as a new endogenous OCT2 substrate related to metformin disposition. PLoS ONE 2012, 7, e36637. [Google Scholar] [CrossRef] [PubMed]
- Fiehn, O.; Wohlgemuth, G.; Scholz, M.; Kind, T.; Lee, D.Y.; Lu, Y.; Moon, S.; Nikolau, B. Quality control for plant metabolomics: Reporting MSI-compliant studies. Plant J. 2008, 53, 691–704. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Mandal, R.; Sinelnikov, I.V.; Broadhurst, D.; Wishart, D.S. MetaboAnalyst 2.0-a comprehensive server for metabolomic data analysis. Nucleic Acids Res. 2012, 40, W127–W133. [Google Scholar] [CrossRef] [PubMed]
- Sample Availability: Samples of the compounds used in the study are available from the authors.
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, D.; Wang, X.; Wu, Y.; Lu, B.; Yuan, A.; Leon, C.; Guo, N. Urinary Metabolomic Profiling Reveals the Effect of Shenfu Decoction on Chronic Heart Failure in Rats. Molecules 2015, 20, 11915-11929. https://doi.org/10.3390/molecules200711915
Yang D, Wang X, Wu Y, Lu B, Yuan A, Leon C, Guo N. Urinary Metabolomic Profiling Reveals the Effect of Shenfu Decoction on Chronic Heart Failure in Rats. Molecules. 2015; 20(7):11915-11929. https://doi.org/10.3390/molecules200711915
Chicago/Turabian StyleYang, Dawei, Xiaoxing Wang, Yaping Wu, Bo Lu, Aifeng Yuan, Carlos Leon, and Na Guo. 2015. "Urinary Metabolomic Profiling Reveals the Effect of Shenfu Decoction on Chronic Heart Failure in Rats" Molecules 20, no. 7: 11915-11929. https://doi.org/10.3390/molecules200711915





