HCN Channels and Heart Rate
Abstract
:1. Introduction
- - An inward current, If, induced by hyperpolarization;
- - An inward current of calcium, ICa;
- - An outward current, Ik.
2. The Sinoatrial Pacemaker Currents
3. The “Funny” Current
4. The HCN Family: The Mediators of the If Current
5. Genetic Mutations of the HCN Channels and Cardiac Arrhythmias
6. Biological Pacemakers
7. HCN Channels, Heart Rate and Pharmacological Interventions
8. HCN Channels and Knock-Out Mice Models: The Experimental Face of HCN Functions
9. Conclusions
Conflicts of Interest
References
- Brown, H.F.; DiFrancesco, D.; Noble, S.J. How does adrenaline accelerate the heart? Nature 1979, 280, 235–236. [Google Scholar]
- DiFrancesco, D.; Ferroni, A.; Mazzanti, M.; Tromba, C. Properties of the hyperpolarizing-activated current sino-atrial node. J. Phisiol. 1986, 377, 61–88. [Google Scholar]
- Difrancesco, D.; Tromba, C. Inhibition of the hyperpolarization-activated current (if) induced by acethylcholine in rabbit sino-atrial node myocytes. J. Phisiol. 1988, 405, 477–491. [Google Scholar]
- Noble, D.; Tsien, R.W. Kinetics of slow component of potassium current in cardiac purkinje fibres. J. Physiol. 1968, 194, 31P–32P. [Google Scholar]
- Draper, M.H.; Weidmann, S. Cardiac resting and action potentials recorded with an intracellular electrode. J. Physiol. 1951, 115, 74–94. [Google Scholar]
- Vassalle, M. Analysis of cardiac pacemaker potential using a “voltage clamp” technique. Am. J. Physiol. 1966, 210, 1335–1341. [Google Scholar]
- DiFrancesco, D. A new interpretation of the pace-maker current in calf Purkinje fibres. J. Physiol. 1981, 314, 359–376. [Google Scholar]
- DiFrancesco, D. A study of the ionic nature of the pace-maker current in calf Purkinje fibres. J. Physiol. 1981, 314, 377–393. [Google Scholar]
- DiFrancesco, D. Pacemaker mechanisms in cardiac tissue. Annu. Rev. Physiol. 1993, 55, 455–472. [Google Scholar]
- Brown, H.; DiFrancesco, D. Voltage-clamp investigations of membrane currents underlying pace-maker activity in rabbit sino-atrial node. J. Physiol. 1980, 308, 331–351. [Google Scholar]
- Yanagihara, K.; Irisawa, H. Inward current activated during hyperpolarization in the rabbit sinoatrial node cell. Pflugers Arch. 1980, 385, 11–19. [Google Scholar]
- DiFrancesco, D.; Ducouret, P.; Robinson, R.B. Muscarinic modulation of cardiac rate at low acetylcholine concentrations. Science 1989, 243, 669–671. [Google Scholar]
- DiFrancesco, D. Characterization of single pacemaker channels in cardiac sino-atrial node cells. Nature 1986, 324, 470–473. [Google Scholar]
- Noble, D.; Denyer, J.C.; Brown, H.F.; DiFrancesco, D. Reciprocal role of the inward currents Ib, Na and If in controlling and stabilizing pacemaker frequency of rabbit sino-atrial node cells. Proc. R. Soc. Lond. B 1992, 250, 199–207. [Google Scholar]
- Ludwig, A.; Zong, X.; Jeglitsch, M.; Hofmann, F.; Biel, M. A family of hyperpolarization-activated mammalian cation channels. Nature 1998, 393, 587–591. [Google Scholar]
- Santoro, B.; Liu, D.T.; Yao, H.; Bartsch, D.; Kandel, E.R.; Siegelbaum, S.A.; Tibbs, G.R. Identification of a gene encoding a hyperpolarization-activated pacemaker channel of brain. Cell 1998, 93, 717–729. [Google Scholar]
- Nof, E.; Antzelevitch, C.; Glikson, M. The Contribution of HCN4 to normal sinus node function in humans and animal models. Pacing. Clin. Electrophysiol. 2010, 33, 100–106. [Google Scholar]
- Shi, W.; Wymore, R.; Yu, H.; Wu, J.; Wymore, R.T.; Pan, Z.; Robinson, R.B.; Dixon, J.E.; McKinnon, D.; Cohen, I.S. Distribution and prevalence of hyperpolarization-activated cation channel (HCN) mRNA expression in cardiac tissues. Circ. Res. 1999, 85, e1–e6. [Google Scholar]
- Shi, W.; Wymore, R.; Yu, H.; Wu, J.; Wymore, R.T.; Pan, Z.; Robinson, R.B.; Dixon, J.E.; McKinnon, D.; Cohen, I.S. Hyperpolarization-activated cyclic nucleotide-gated channel 1 is a molecular determinant of the cardiac pacemaker current If. J. Biol. Chem. 2001, 276, 29233–29241. [Google Scholar]
- Altomare, C.; Terragni, B.; Brioschi, C.; Milanesi, R.; Pagliuca, C.; Viscomi, C.; Moroni, A.; Baruscotti, M.; DiFrancesco, D. Heteromeric HCN1-HCN4 channels: A comparison with native pacemaker channels from the rabbit sinoatrial node. J. Physiol. 2003, 549, 347–359. [Google Scholar]
- DiFrancesco, D.; Tortora, P. Direct activation of cardiac pacemaker channels by intracellular cyclic AMP. Nature 1991, 351, 145–147. [Google Scholar]
- DiFrancesco, D.; Mangoni, M. Modulation of single hyperpolarization-activated channels (i(f)) by cAMP in the rabbit sino-atrial node. J. Physiol. 1994, 474, 473–482. [Google Scholar]
- DiFrancesco, D. Dual allosteric modulation of pacemaker (f) channels by cAMP and voltage in rabbit SA node. J. Physiol. 1999, 515, 367–376. [Google Scholar]
- Barbuti, A.; Gravante, B.; Riolfo, M.; Milanesi, R.; Terragni, B.; DiFrancesco, D. Localization of pacemaker channels in lipid rafts regulates channel kinetics. Circ. Res. 2004, 94, 1325–1331. [Google Scholar]
- Barbuti, A.; Terragni, B.; Brioschi, C.; DiFrancesco, D. Localization of f-channels to caveolae mediates specific beta2-adrenergic receptor modulation of rate in sinoatrial myocytes. J. Mol. Cell Cardiol. 2007, 42, 71–78. [Google Scholar]
- Milanesi, R.; Baruscotti, M.; Gnecchi-Ruscone, T.; DiFrancesco, D. Familial sinus bradycardia associated with a mutation in the cardiac pacemaker channel. N. Engl. J. Med. 2006, 354, 151–157. [Google Scholar]
- Baruscotti, M.; Bottelli, G.; Milanesi, R.; DiFrancesco, J.C.; DiFrancesco, D. HCN-related channelopathies. Pflugers Arch. 2010, 460, 405–415. [Google Scholar]
- Nof, E.; Luria, D.; Brass, D.; Marek, D.; Lahat, H.; Reznik-Wolf, H.; Pras, E.; Dascal, N.; Eldar, M.; Glikson, M. Point mutation in the HCN4 cardiac ion channel pore affecting synthesis, trafficking, and sinus bradycardia. Circulation 2007, 116, 463–470. [Google Scholar]
- Schulze-Bahr, E.; Neu, A.; Friederich, P.; Kaupp, U.B.; Breithardt, G.; Pongs, O.; Isbrandt, D. Pacemaker channel dysfunction in a patient with sinus node disease. J. Clin. Invest. 2003, 111, 1537–1545. [Google Scholar]
- Ueda, K.; Nakamura, K.; Hayashi, T.; Inagaki, N.; Takahashi, M.; Arimura, T.; Morita, H.; Higashiuesato, Y.; Hirano, Y.; Yasunami, M.; Takishita, S.; Yamashina, A.; Ohe, T.; Sunamori, M.; Hiraoka, M.; Kimura, A. Functional characterization of a trafficking-defective HCN4 mutation, D553N, associated with cardiac arrhythmia. J. Biol. Chem. 2004, 279, 27194–27198. [Google Scholar]
- Rosen, M.R.; Robinson, R.B.; Brink, P.R.; Cohen, I.S. The road to biological pacing. Nat. Rev. Cardiol. 2011. [Google Scholar] [CrossRef]
- Robinson, R.B. Engineering a biological pacemaker: In vivo, in vitro and in silico models. Drug Discov. Today Dis. Models 2009, 6, 93–98. [Google Scholar] [CrossRef]
- Beere, P.A.; Glagov, S.; Zarins, C.K. Retarding effect of lowered heart rate on coronary atherosclerosis. Science 1984, 226, 180–182. [Google Scholar]
- Heidland, U.E.; Strauer, B.E. Left ventricular muscle mass and elevated heart rate are associated with coronary plaque disruption. Circulation 2001, 104, 1477–1482. [Google Scholar]
- Yusuf, S.; Camm, A.J. Sinus tachyarrhythmias and the specific bradycardic agents: A marriage made in heaven? J. Cardiovasc. Pharmacol. Ther. 2003, 8, 89–105. [Google Scholar] [CrossRef]
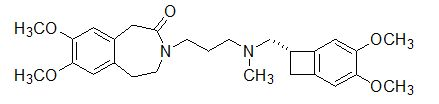
- DiFrancesco, D.; Camm, J.A. Heart rate lowering by specific and selective if current inhibition with ivabradine: A new therapeutic perspective in cardiovascular disease. Drugs 2004, 64, 1757–1765. [Google Scholar]
- DiFrancesco, D. The pacemaker current (If) plays an important role in regulating SA node pacemaker activity. Cardiovasc. Res. 1995, 30, 307–308. [Google Scholar]
- Vassalle, M. The pacemaker current (If) does not play an important role in regulating SA node pacemaker activity. Cardiovasc. Res. 1995, 30, 309–310. [Google Scholar]
- Kobinger, W.; Lillie, C.; Pichler, L. N-Allyl-derivative of clonidine, a substance with specific bradycardic action at a cardiac site. Naunyn. Schmiedebergs Arch. Pharmacol. 1979, 306, 255–262. [Google Scholar] [CrossRef]
- Lillie, C.; Kobinger, W. Comparison of the bradycardic effects of alinidine (St 567), AQ-A 39 and verapamil on guinea-pig sinoatrial node superfused with different Ca2+ and NaCl solutions. Eur. J. Pharmacol. 1983, 87, 25–33. [Google Scholar]
- Traunecker, W.; Walland, A. Haemodynamic and electrophysiologic actions of alinidine in the dog. Arch. Int. Pharmacodyn. Ther. 1980, 244, 58–72. [Google Scholar]
- Millar, J.S.; Williams, E.M. Pacemaker selectivity: Influence on rabbit atria of ionic environment and of alinidine, a possible anion antagonist. Cardiovasc. Res. 1981, 15, 335–350. [Google Scholar]
- Van Bogaert, P.P.; Pittoors, F. Use-dependent blockade of cardiac pacemaker current (If) by cilobradine and zatebradine. Eur. J. Pharmacol. 2003, 478, 161–171. [Google Scholar]
- DiFrancesco, D. Some properties of the UL-FS 49 block of the hyperpolarization-activated current (If) in sino-atrial node myocytes. Pflugers Arch. 1994, 427, 64–70. [Google Scholar]
- Bois, P.; Bescond, J.; Renaudon, B.; Lenfant, J. Mode of action of bradycardic agent, S 16257, on ionic currents of rabbit sinoatrial node cells. Br. J. Pharmacol. 1996, 118, 1051–1057. [Google Scholar]
- Bucchi, A.; Baruscotti, M.; DiFrancesco, D. Current-dependent block of rabbit sino-atrial node If channels by ivabradine. J. Gen. Physiol. 2002, 120, 1–13. [Google Scholar]
- Köster, R.; Kaehler, J.; Meinertz, T. Treatment of stable angina pectoris by ivabradine in every day practice: the REDUCTION study. Am. Heart J. 2009, 158, e51–e57. [Google Scholar]
- Fox, K.; Ford, I.; Steg, P.G.; Tendera, M.; Ferrari, R. BEAUTIFUL Investigators. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): A randomised, double-blind, placebo-controlled trial. Lancet 2008, 372, 807–816. [Google Scholar] [CrossRef]
- Fox, K.; Ford, I.; Steg, P.G.; Tendera, M.; Robertson, M.; Ferrari, R. BEAUTIFUL investigators. Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): A subgroup analysis of a randomised controlled trial. Lancet 2008, 372, 817–821. [Google Scholar] [CrossRef]
- Ekman, I.; Chassany, O.; Komajda, M.; Böhm, M.; Borer, J.S.; Ford, I.; Tavazzi, L.; Swedberg, K. Heart rate reduction with ivabradine and health related quality of life in patients with chronic heart failure: results from the SHIFT study. Eur. Heart J. 2011, 32, 2395–2404. [Google Scholar]
- Mulder, P.; Barbier, S.; Chagraoui, A.; Richard, V.; Henry, J.P.; Lallemand, F.; Renet, S.; Lerebours, G.; Mahlberg-Gaudin, F.; Thuillez, C. Long-term heart rate reduction induced by the selective If current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failure. Circulation 2004, 109, 1674–1679. [Google Scholar]
- Custodis, F.; Baumhäkel, M.; Schlimmer, N.; List, F.; Gensch, C.; Böhm, M.; Laufs, U. Heart rate reduction by ivabradine reduces oxidative stress, improves endothelial function, and prevents atherosclerosis in apolipoprotein E-deficient mice. Circulation 2008, 117, 2377–2387. [Google Scholar]
- Heusch, G.; Skyschally, A.; Gres, P.; van Caster, P.; Schilawa, D.; Schulz, R. Improvement of regional myocardial blood flow and function and reduction of infarct size with ivabradine: Protection beyond heart rate reduction. Eur. Heart J. 2008, 29, 2265–2275. [Google Scholar]
- Nof, E.; Antzelevitch, C.; Glikson, M. The Contribution of HCN4 to Normal Sinus Node Function in Humans and Animal Models. Pacing. Clin. Electrophysiol. 2010, 33, 100–106. [Google Scholar]
- Baruscotti, M.; Bucchi, A.; Viscomi, C.; Mandelli, G.; Consalez, G.; Gnecchi-Rusconi, T.; Montano, N.; Rabello Casali, K.; Micheloni, S.; Barbuti, A.; DiFrancesco, D. Deep bradycardia and heart block caused by inducible cardiac-specific knockout of the pacemaker canne gene Hcn4. Proc. Natl. Acad. Sci. USA 2011, 108, 1705–1710. [Google Scholar]
- Herrmann, S.; Stieber, J.; Stockl, J.; Hofmann, F.; Ludwig, A. HCN4 provides a ‘depolarization reserve’ and is not required for heart rate acceleration in mice. EMBO J. 2007, 26, 4423–4432. [Google Scholar]
- Stieber, J.; Herrmann, S.; Feil, S.; Löster, J.; Feil, R.; Biel, M.; Hofmann, F.; Ludwig, A. The hyperpolarization-activated channel HCN4 is required for the generation of pacemaker action potentials in the embryonic heart. Proc. Natl. Acad. Sci. USA 2003, 100, 15235–15240. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Scicchitano, P.; Carbonara, S.; Ricci, G.; Mandurino, C.; Locorotondo, M.; Bulzis, G.; Gesualdo, M.; Zito, A.; Carbonara, R.; Dentamaro, I.; et al. HCN Channels and Heart Rate. Molecules 2012, 17, 4225-4235. https://doi.org/10.3390/molecules17044225
Scicchitano P, Carbonara S, Ricci G, Mandurino C, Locorotondo M, Bulzis G, Gesualdo M, Zito A, Carbonara R, Dentamaro I, et al. HCN Channels and Heart Rate. Molecules. 2012; 17(4):4225-4235. https://doi.org/10.3390/molecules17044225
Chicago/Turabian StyleScicchitano, Pietro, Santa Carbonara, Gabriella Ricci, Cosimo Mandurino, Manuela Locorotondo, Gabriella Bulzis, Michele Gesualdo, Annapaola Zito, Rosa Carbonara, Ilaria Dentamaro, and et al. 2012. "HCN Channels and Heart Rate" Molecules 17, no. 4: 4225-4235. https://doi.org/10.3390/molecules17044225